-
 Injury keeping you out of the game?Our experts will get to the core of your fitness needs.OUR SERVICES
Injury keeping you out of the game?Our experts will get to the core of your fitness needs.OUR SERVICES -
 GET BACK TO THE ACTIVITIES YOU LOVEOUR SERVICES
GET BACK TO THE ACTIVITIES YOU LOVEOUR SERVICES -
 RESTORING YOUR PHYSICAL ABILITYOUR SERVICES
RESTORING YOUR PHYSICAL ABILITYOUR SERVICES -
 RESTORING YOUR QUALITY OF LIFEOUR SERVICES
RESTORING YOUR QUALITY OF LIFEOUR SERVICES -
 EVIDENCE BASED PRACTICEOUR SERVICES
EVIDENCE BASED PRACTICEOUR SERVICES -
 APPROPRIATE PROGRAM FOR A SUCCESSFUL RECOVERYOUR SERVICES
APPROPRIATE PROGRAM FOR A SUCCESSFUL RECOVERYOUR SERVICES -
 HELPING YOU ACHIEVE YOUR GOALSOUR SERVICES
HELPING YOU ACHIEVE YOUR GOALSOUR SERVICES
Ankle
An ankle fracture occurs when a bone on 1 or both sides of the ankle is partially or completely broken. Most ankle fractures are caused by twisting injuries and falls, or injuries experienced during sports or play. Under the age of 50, most ankle fractures occur in men. Over the age of 50, women experience more ankle fractures. The type of fracture varies from simple to complex, and can involve 1 or all 3 bones that make up the ankle joint. It is important to seek treatment after an ankle injury to determine if you have a fracture. Physical therapy shares an important role in your treatment and recovery from an ankle fracture, for a return to normal activity.
What is an Ankle Fracture?
An ankle fracture is a completely or partially broken bone on 1 or both sides of the ankle joint. There are several types of ankle fractures, and 1, 2, or 3 bones may be fractured. The classifications based on the number of bones broken are:
- Lateral malleolus fracture. Only the bone on the outside of the ankle, the fibula, is broken.
- Medial malleolus fracture. Only the bone on the inside of the ankle, the tibia, is broken.
- Bi-malleolar fracture. Two bones are broken, the fibula and the tibia.
- Trimalleolar fracture. Three bones are broken, the fibula, tibia, and the posterior malleolus (the tibia at the back of the foot).
The severity of the fracture is classified as:
- Nondisplaced. The pieces of the fractured bone remain lined up.
- Displaced. The 2 parts of the fractured bone do not line up.
- Comminuted. Splinters or multiple small pieces of bone are found at the fracture site.
- Complex Fracture. The soft tissue surrounding the broken bone is severely damaged.
- Compound Fracture. Fracture fragments can pierce the skin.
When a fracture involves several broken bones or the bones do not remain lined up, the fracture is considered to be unstable and requires immediate treatment. A compound fracture also involves a risk of infection.
Signs and Symptoms
People who fracture their ankles may experience:
- Immediate, severe pain after a twisting injury or fall.
- A “pop” or “snap” felt or heard at the time of the injury.
- Swelling in the ankle.
- Tenderness or pain in the ankle area.
- Difficulty bearing weight on the ankle when standing, walking.
- Not being able to bear weight on the ankle at all.
- Bruising.
- Pain that increases with activity and improves with rest.
- Inability to put a shoe on due to swelling and pain.
- A bump or deformity that may be seen or felt at the ankle.
How Is It Diagnosed?
If you see your physical therapist after an ankle injury, the physical therapist will ask about your medical history, and how the injury occurred. Your physical therapist will observe your ability to walk and bear weight on the injured side, and gently examine the area to observe any swelling, deformity, and tenderness. Your physical therapist also will examine your foot and lower leg to identify whether other areas may be injured. If a fracture is suspected, your physical therapist will consult with your physician. An x-ray is needed to confirm or rule out an ankle fracture. You may then be referred to an orthopedic physician or emergency room for further treatment.
It is important to have an ankle injury assessed by your physical therapist or medical provider soon after an ankle injury, to distinguish a severe sprain from a broken bone.
How Can a Physical Therapist Help?
Before Surgery
If you see your physical therapist after your injury and an ankle fracture is suspected, your physical therapist will:
- Instruct you in acute injury care using the RICE formula: rest, ice, compression, and elevation.
- Immobilize your ankle by wrapping it with an ace wrap, or applying a stirrup brace to limit motion and control swelling.
- Apply ice to reduce pain and swelling.
- Instruct you to keep the involved ankle elevated to control swelling.
- Instruct you to walk without putting weight on the injured ankle, using crutches or a walker.
- Make recommendations for additional care with an orthopedic physician or emergency department.
If you have an ankle fracture, treatment will depend on how many bones are broken, and if it is a simple, complex, or compound fracture. Initial treatment involves the realigning and stabilizing of the bones by your physician, and is performed in the hospital emergency room or, if needed, with surgery.
After Surgery
If surgery is required, the affected ankle will be placed in a cast or fracture boot to stabilize it following surgery. A physical therapist will visit your hospital room once you are medically stable, to help you get up and out of bed. Your physical therapist will help you sit up on the bedside, and then stand up. You will not be allowed to put any weight on the involved ankle for about 6 to 10 weeks. Your physical therapist will teach you how to walk with the use of an assistive device, such as crutches or a walker. You will also learn how to go up and down steps and curbs using your assistive device.
When an x-ray confirms that the fracture has healed, your physician will remove your cast. Your physical therapist will work with you to safely put weight on your ankle, and begin treatment to help you return to your normal activity.
If You Do Not Require Surgery
A physical therapist can help treat a broken ankle after it has been treated by a physician and immobilized. After the bone is healed, a physical therapist can help you gain back your strength, motion, balance, and sport skills.
After your injured leg is placed in a cast or a cast boot, your physical therapist will teach you how to walk without bearing weight on the injured ankle, using crutches or a walker. Your physical therapist will teach you how to get in and out of bed, and your car. Your physical therapist will provide you with the equipment that best suits your needs.
When healing of the fracture is seen on an x-ray, your physician will remove your cast, and you will begin bearing weight on that leg again, and continue your physical therapy treatment.
Physical therapy treatment will include:
- Walking Instruction. Your physical therapist will help you begin to put some of your weight on the injured leg, gradually progressing to full weight as your physician recommends.
- Gait Training. Your physical therapist will offer specific instruction and exercises to restore a normal walking pattern. The focus will be on how your foot and ankle move, and the timing of your steps. You may practice on a treadmill at low speed, on level ground, and on steps.
- Reducing Swelling. Swelling is common after an ankle fracture. Treatment may include gentle massage, the use of a compression wrap, ice, or heat, and elevating the affected ankle when at rest.
- Exercise. Your physical therapist will design an exercise plan to begin when the cast is removed to help you strengthen and regain motion in your injured ankle. It is important to regain the ability to bend your ankle to restore your full walking ability.
- Restoring Ankle Mobility. Your physical therapist may use manual (hands-on) therapy to gently move your foot and ankle joints and surrounding tissues to reduce stiffness, and increase the ankle's bending range of motion.
- Return to Work/Play Activity. As you regain strength and flexibility, your physical therapist will provide activity training specific to your job, leisure activity, or sport.
Return to full participation in sports and work activities generally occurs 12 to 16 weeks after an ankle fracture.
Note: Physical therapy treatment is different for each person and depends on your type of injury, how you are healing, and whether you had surgery, as well as your age and physical health.
Can this Injury or Condition be Prevented?
Not all ankle fractures can be prevented. However, some precautions may be taken.
To reduce your risk of ankle injury:
- Wear appropriate protective gear when participating in sports.
- Train to reach your top strength and fitness levels.
- Wear proper shoes, and replace athletic shoes regularly.
To reduce your fall risk:
- Remove obstacles and clutter from hallways and rooms in your home.
- Work and play in well-lighted areas.
- Use night lights in the home.
- Install grab bars to tub/shower areas.
- Add railings to both sides of stairways.
- Maintain strength and fitness throughout your life.
Ankle sprains are common injuries that occur when the foot twists or turns beyond its normal range of movement, causing the ligaments of the ankle to overstretch or tear. It is estimated that 23,000 Americans experience ankle sprains daily. Of all sports injuries in the United States, 45% are ankle sprains; basketball players are the athletes most often affected. People who have an increased risk of spraining an ankle include younger athletes, members of the military, and anyone who frequently runs, jumps, and changes direction quickly, while performing an athletic activity (“cutting motion”). Physical therapists help people who have experienced ankle sprains reduce their pain; regain their strength, motion, and balance; return to normal activity levels; and avoid reinjury.
What Is an Ankle Sprain?
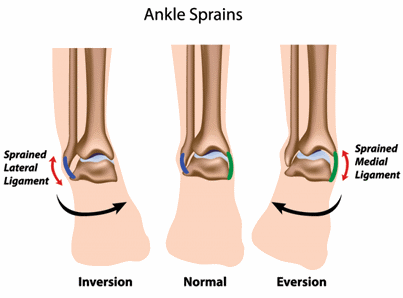
Sprains are injuries to ligaments (the bands of tissue that hold joints together). Ankle sprains occur when the foot twists or turns beyond its normal range of movement, causing the ligaments connecting the bones of the leg, ankle, and foot to overstretch or tear.
The ligaments on the outer (lateral) side of the ankle are the ones most commonly injured. Ligaments on the inner (medial) side of the ankle, or above the ankle bone, can also be sprained, but are injured less frequently.
An ankle sprain usually takes between 2 weeks to 2 months to heal. The ankle will feel better after a few weeks, and be fully strengthened in a few months. A severely sprained ligament, however, can take 9 months to 1 year to heal.
Recurrent ankle sprains are common; once an ankle ligament is sprained, it is often reinjured. In fact, 73% of people who have sprained an ankle once are likely to do so again. Reinjury is especially likely if muscle strength and balance are not fully restored to, or improved beyond, preinjury levels.
How Does it Feel?
Right after an ankle sprain, you may experience:
- Pain
- Swelling
- Inability to stand or walk on the affected foot
- Throbbing
- Stiffness
- Weakness
- A feeling of instability in the ankle joint
After most sprains, you feel pain right away at the site of the ligament stretch or tear. Often, the ankle starts to swell immediately and may bruise. The ankle area usually is tender to the touch, and when you move the ankle, it hurts. In more severe sprains, you may hear or feel something tear, along with a "pop" or "snap."
How Is It Diagnosed?
If you see your physical therapist first, the physical therapist will examine your ankle, take your health history, and ask questions such as:
- How did you get injured?
- Did you feel a pop, snap, or tear?
- What activities are you having trouble doing?
- What activities do you want to get back to doing?
Your physical therapist will gently press around your ankle to see if it is painful to the touch, and may use additional tests to determine if other parts of your foot are injured. Your physical therapist will test your strength and flexibility, observe how you can move your foot and leg, and watch how you walk.
Depending on how badly a ligament is damaged, or how many ligaments are injured, your ankle sprain may be classified as:
- Grade 1 (mild). The ligament is overstretched.
- Grade 2 (moderate). The ligament is overstretched or partially torn.
- Grade 3 (severe). The ligament is completely torn.
Your physical therapist also will test and screen for other, more serious conditions that could be causing the pain and swelling. To provide a definitive diagnosis, your physical therapist may collaborate with an orthopedic physician or other health care provider, who may order further tests, such as an x-ray, to confirm the diagnosis and to rule out other damage to the ankle, including a fracture.
How Can a Physical Therapist Help?
Physical therapists help people with ankle sprains recover more quickly than they would without treatment. The time it takes to heal an ankle sprain varies, but results can often be achieved in 2 to 8 weeks. Your physical therapist will work with you to design a specific treatment program that meets your needs and goals.
During the first 24 to 48 hours following your diagnosis, your physical therapist may advise you to:
- Rest the area by avoiding any activity that causes pain.
- Apply ice packs to the area for 15 to 20 minutes every 2 hours.
- Consult with a physician for further services, such as medication or diagnostic tests.
- Walk on the affected foot as soon, and as much as you are able, without making the pain or swelling worse.
- Use crutches or other walking aids to help alleviate pain and support balance.
- Wrap your ankle or use an ankle brace for support and to prevent swelling.
These self-treatments will allow you to be as active as possible with the least amount of pain, and will help speed healing.
Your physical therapist will work with you to:
Reduce Pain and Swelling. You will learn how to avoid or modify your daily and sports activities to allow healing to begin. Your physical therapist may use different types of treatments and technologies to control and reduce your pain and swelling, including ice, heat, ultrasound, electrical stimulation, taping, specific exercises, and hands-on therapy, such as specialized massage.
Improve Motion. Your physical therapist will choose specific activities and treatments to help restore normal movement in the ankle. These might begin with "passive" motions that the physical therapist performs for you to gently move your ankle and foot, and progress to “active” exercises and stretches that you do yourself.
Improve Flexibility. Your physical therapist will determine if any foot, ankle, or lower leg muscles are tight, begin to stretch them, and teach you how to stretch them.
Improve Strength. Ankle sprains may be related to weak, injured, or uncoordinated leg muscles. Certain exercises will aid healing at each stage of recovery; your physical therapist will choose and teach you the correct exercises and equipment to use, to steadily and safely restore your strength. These may include using cuff weights, stretch bands, and weight-lifting equipment.
Improve Endurance. Regaining your muscular endurance in the ankle and leg is important after an injury. Your physical therapist will teach you exercises to improve endurance, so you can return to your normal activities. Cardio-exercise equipment may be used, such as treadmills or stationary bicycles.
Improve Balance. Regaining your sense of balance is important after an injury. Your physical therapist will teach you exercises to improve your balance ability.
Restore Agility. Speed and accuracy of leg movement is important in athletics and in many daily activities. Your physical therapist will help you regain these skills in preparation for a return to sports and to your daily routine.
Learn a Home Program. Your physical therapist will teach you strengthening and stretching exercises to perform at home. These exercises will be specific for your needs; if you do them as prescribed by your physical therapist, you can speed your recovery.
Return to Activities. Your physical therapist will discuss activity goals with you and use them to set your work, sport, and home-life recovery goals. Your treatment program will help you reach your goals in the safest, fastest, and most effective way possible. Your physical therapist will teach you exercises, work retraining activities, and sport-specific techniques and drills to help you achieve your goals.
Speed Recovery Time. Your physical therapist is trained and experienced in choosing the best treatments and exercises to help you safely heal, return to your normal lifestyle, and reach your goals faster than you are likely to do on your own.
If Surgery Is Necessary
Surgery is not commonly required for ankle sprains. But if surgery is needed, you will follow a recovery program over several weeks, guided by your physical therapist. Your physical therapist will help you minimize pain, regain motion and strength, and return to normal activities in the safest and speediest manner possible.
Can this Injury or Condition be Prevented?
Your physical therapist can recommend a home-exercise program to help prevent ankle sprains. It may include strength, flexibility, and balance exercises. If you have sprained your ankle once, it is at greater risk for reinjury in the future, if the ligaments did not heal properly or if your ankle never returned to its normal strength. And if you return to sports or other activities too soon after injury, your ankle might give you persistent pain or might easily or frequently reinjure.
Possible other factors that may increase someone’s risk of spraining an ankle are body weight, female gender, muscle weakness, balance problems, or foot/ankle problems.
To help prevent an ankle sprain or a reinjury, your physical therapist may recommend that you:
- Warm up effectively before athletic activities.
- Use footwear that is best for specific activities.
- Use ankle wraps or braces as directed.
- Perform specific balance and strength exercises several times per week for up to a year.
- Maintain a healthy body weight.
Ankle impingement occurs when either soft or bony tissues are compressed within the ankle joint at the extreme end of a motion, such as pointing the foot sharply downward. It typically affects people who experience forces through their ankle at these "end-range" positions, such as dancers, gymnasts, or people performing kicking activities. Additionally, people who perform repetitive tasks that involve squatting or stair-climbing are susceptible to this condition. Physical therapists help people with ankle impingement reduce their pain, heal and strengthen the affected area, and improve their overall balance.
What is Ankle Impingement?
Ankle impingement can be categorized into 2 types:
- Anterior ankle impingement
- Posterior ankle impingement
Anterior ankle impingement involves pain on the front side of your ankle. Inflammation and swelling occur due to repetitive stresses at end-range positions of the ankle, such as when one jumps, squats, or descends stairs. These may eventually lead to development of bone spurs (a bony overgrowth) in the ankle joint space. An additional cause of anterior ankle impingement is ankle instability. Ankle instability is a looseness of the ankle joint that develops after repeated ankle sprains, causing damage to ligaments in the ankle. This damage can cause the ligaments to become scarred and take up more joint space. Tissue in the joint space is then compressed, causing pain during activities that require ankle dorsiflexion (stretching your toes up toward your shin). Examples of these activities include squatting, jumping, and stair-climbing.
Posterior ankle impingement involves pain on the back side of your ankle, especially during activities that involve pointing your toes. The pain is caused by compression of soft or bony tissue between the shin bone (tibia) and the heel bone (calcaneus). Some people have a small extra bone in the back of their ankle called the Os Trigonum. This little bone can lead to posterior impingement because of compression between the shin bone and the heel bone, when the foot is pointed. Additionally, large amounts of force on the ankle occasionally may cause small pieces to break off the ankle bone, which can also become compressed when the ankle moves into "end-range plantar flexion" (moving the foot or toes downward toward the sole of the foot). Compression of tissue causes inflammation and swelling that leads to pain.
Signs and Symptoms
With anterior ankle impingement, you may experience:
- Pain on the front and/or outside of the ankle joint
- A feeling of ankle instability
- Decreased ankle range of motion when stretching your toes up toward your shin
- Pain at the end-range of stretching your toes toward your shin
- Tenderness at the front of the ankle when touched
With posterior ankle impingement, you may experience:
- Pain on the back of your ankle, especially during activities that involve pointing your toes
- Decreased range of motion when pointing your toes
- Tenderness on the back of the ankle when touched
How Is It Diagnosed?
Your examination will begin with your personal health history and current symptoms. Your physical therapist will ask you when your symptoms began, where the location of your pain is, and what activities cause you pain. Your physical therapist will perform a physical examination to evaluate your ankle strength, range of motion, sensation, and structural stability as well as your balance. Your physical therapist also will perform special tests, such as gently moving your ankle to see if it causes symptoms.
To diagnose posterior ankle impingement in dancers, the exam may be specialized to that activity. For example, a physical therapist may ask a ballet dancer to demonstrate the “en pointe” position, which involves standing on the tips of the toes.
To provide a definitive diagnosis, your therapist may collaborate with an orthopedist or other health care provider. The most accurate method to diagnose ankle impingement is by X-ray or magnetic resonance imaging (MRI), which can be ordered by the orthopedist.
How Can a Physical Therapist Help?
Once you have been diagnosed with ankle impingement, your physical therapist will work with you to achieve your functional goals, and help you return to activities you previously performed without pain. Your treatment may include:
Pain Management. Your physical therapist may use ice massage or electrical stimulation, if you have inflammation causing pain. Your physical therapist may ask you to reduce your activity level for a while, so the inflammation in your ankle can decrease.
Range-of-Motion Exercises. Your physical therapist may gently move your ankle through its available range of motion, or teach you the proper motions to move through in order to increase its mobility and decrease stiffness. If necessary, your physical therapist may perform joint mobilizations—skillfully moving the joint in a particular direction to improve its motion.
Muscle-Strengthening Exercises. It is important to strengthen the muscles acting on the foot, ankle, and lower leg to promote proper joint mechanics. When the muscles are strong and working properly, the joint space in the ankle is maintained, which decreases the risk of compression of soft or bony tissues.
Balance Exercises. Your physical therapist may give you balance exercises to challenge the way your body reacts to outside forces. These exercises make you more aware of where your body is in space. Improving your balance will lead to a more stable ankle, because your body can more easily respond to challenges.
Functional Training. Once your physical therapist has helped decrease your ankle pain and inflammation, you will progress to more activity-specific tasks. Your physical therapist will help ensure that your ankle can withstand challenges during occupational, sport, or artistic activities.
Can this Injury or Condition be Prevented?
No injury is ever completely preventable. However, there are some actions that active and at-risk people can take to reduce the risk of ankle impingement, including:
- Using correct techniques when performing physical activities.
- Wearing proper footwear; eg, basketball players can wear high-top shoes to improve their ankle stability.
- Avoiding overtraining; conditions like ankle impingement tend to be brought on by repetitive stresses.
Overuse injuries in sports account for 50% of all injuries. A majority of overuse injuries occur in runners, with 20% of injuries affecting the lower leg, 15% the ankle, and 15% the foot.
Peroneal tendinopathy is a type of overuse injury that often occurs in athletes, like long-distance runners and basketball players. Dancers, people who have had ankle sprains, or those who simply have weak ankles are also often affected. Peroneal tendinopathy is characterized by an aching along the outside surface of the ankle that worsens with activity, yet improves with rest. A physical therapist can help relieve symptoms caused by this condition by providing treatments, including stretching and strengthening exercises to help the ankle become more mobile, strong, and stable.
What is Peroneal Tendinopathy?
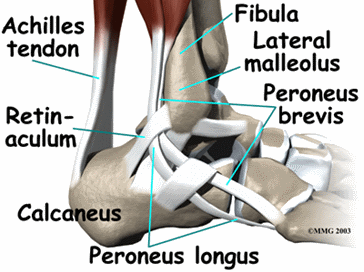
Peroneal tendinopathy is characterized by an aching pain and swelling in the peroneal tendons located in the lower, outside portion of the ankle. A tendon is soft-tissue that attaches a muscle to a bone. The muscles involved in this condition are the 2 peroneal muscles in the lower leg, called the peroneus longus and the peroneus brevis. (In some texts, the muscles are referred to as the fibularis longus and the fibularis brevis.)
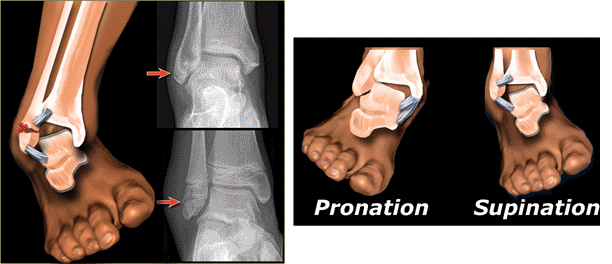
The peroneus longus muscle originates on the fibula bone, which is located on the outside of the lower leg. It wraps around the bone on the outside of the ankle (the lateral malleolus) and attaches to the plantar (bottom) aspect of the base of the big toe. The peroneus brevis muscle also originates on the fibula, but attaches to the base of the fifth toe. These muscles are responsible for moving the foot in an outward direction, and pointing the toe and foot downward. Together, they help to balance and stabilize the foot and ankle. Most ankle sprains occur as a result of the ankle rolling inward. One reason for this is that the peroneal muscles and tendons are not as strong as the muscles on the inside of the ankle. If these muscles are weak, they may not be able to prevent the ankle from rolling inward. These muscles and tendons can also be overworked if the foot isn’t hitting the ground in proper alignment. If the foot hits the ground more on the outside of the foot (supination), the peroneal muscles have to work harder to stabilize the force of gravity with weight-bearing activities. Proper footwear or orthotics can help with proper foot alignment.
Peroneal tendinopathy will usually worsen with activity, such as running or walking and improve with rest. It is an overuse injury, meaning the tendons can become enlarged, thickened, and possibly swollen.
How Does it Feel?
Symptoms of peroneal tendinopathy include:
- An aching pain on the outside of the ankle, especially with activity
- Lateral (outside) ankle pain that decreases with rest
- Swelling or tenderness to touch behind the ankle bone on the outside of the ankle
- Pain and weakness when actively moving the foot in an outward direction or when pointing it down
- Pain when pushing off the ball of the foot during walking or running
- Pain when walking on a sloped terrain that turns the foot outward
- Pain when stretching the foot in an inward and downward direction
How Is It Diagnosed?
Your physical therapist will conduct a thorough evaluation that includes asking about your health history. Your physical therapist may perform strength and motion tests on your ankle, ask about your job duties and hobbies, evaluate your gait (how you walk), and check for any muscle weakness in the entire leg and in your core. Your therapist will also check your posture and evaluate what type of shoes you wear to determine if they support your foot properly. Your physical therpist will gently touch your ankle in specific areas to determine which tendon or tendons may be inflamed. Special tests may be performed to determine exactly which tendons are involved.
How Can a Physical Therapist Help?
It is important to get proper treatment for peroneal tendinopathy as soon as it occurs. A degenerated tendon that is not treated can begin to tear, causing a more serious condition. With an early diagnosis, physical therapy can successfully treat peroneal tendinopathy. Your physical therapist will develop a treatment plan specific to your condition and goals. Your individual treatment program may include:
Pain Management. Your physical therapist will help you identify and avoid painful movements, allowing the inflamed tendon to heal. Ice, ice massage, or moist heat may be used for pain management. Therapeutic modalities, such as iontophoresis (medication delivered through an electrically charged patch) and ultrasound may be applied.
Manual Therapy. Your physical therapist may use manual therapy (hands-on) techniques to gently mobilize the joints in your foot, ankle, and lower leg. Soft-tissue mobilizations may also be performed to loosen any tightness, increase circulation, and relieve pain and swelling.
Range-of-Motion Exercises. You will learn exercises to help the ankle, foot, and toes to move properly, in order to normalize your gait pattern when walking or running. Stretching exercises will help ease any tightness in the calf muscles and the tissues in the bottom of the foot.
Strengthening Exercises. Your physical therapist will determine which muscle groups require strengthening to enable you to return to walking or running without pain. Navigating uneven surfaces, such as grass, sand, gravel, or trails requires significant ankle strength to avoid unnecessary stress on the ankle. Your physical therapist may teach you to perform resistance exercises with bands, weights, or medicine balls to strengthen the muscles in the ankle, foot, and lower leg.
Functional Training. As your symptoms improve, your physical therapist will help you return to your previous level of activity and sport. Sport-specific exercises will simulate certain activities. You may perform single-leg balance exercises or train on uneven surfaces to challenge the muscles that balance and stabilize the ankle. Your physical therapist will design an individual home-exercise program to perform after formal therapy has ended, to continue building your ankle and foot strength.
Patient Education: Your physical therapist will recommend proper footwear for the activities you enjoy, so that your foot and ankle have proper support. It may be necessary to get fitted for a custom foot orthotic (corrective inserts for your shoes) to wear, especially when performing more demanding activities, such as running or walking on uneven surfaces. You will also learn how to gradually increase and maintain your training regimen to reduce any chance of future injury.
Can this Injury or Condition be Prevented?
Peroneal tendinopathy can be prevented by:
- Keeping the entire leg strong and flexible, including the hip, knee, and ankle.
- Choosing proper footwear for running and walking activities.
- Slowly increasing your running and walking mileage or speed.
- Gradually adding hills or uneven terrain to your exercise route.
- Changing footwear when necessary to properly support the foot.
Plantar fasciitis is a condition causing heel pain. Supporting the arch, the plantar fascia, a thick band of tissue connecting the heel to the ball of the foot, can become inflamed or can tear. You experience pain when you put weight on your foot—particularly when taking your first steps in the morning. The pain can be felt at the heel, or along the arch and the ball of the foot.
Plantar fasciitis is a common foot condition. It occurs in as many as 2 million Americans per year and 10% of the population over their lifetimes.
Factors that contribute to the development of plantar fasciitis include:
- Age (over 40 years)
- A job, sport, or hobby that involves prolonged standing or other weight-bearing activity
- Rapid increases in length or levels of activity, such as beginning a new running program or changing to a job that requires a lot more standing or walking than you are accustomed to
- Decreased calf muscle flexibility
- Increased body weight (Body Mass Index greater than 30)
- Tendency to have a flat foot (pronation)
Plantar fasciitis affects people of all ages, both athletes and non-athletes. Men and women have an equal chance of developing the condition.
Treatment generally reduces pain and restores your ability to put weight on your foot again.
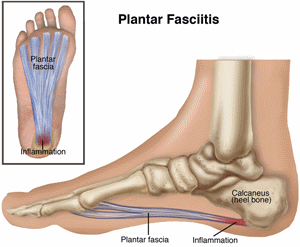
What is Plantar Fasciitis?
Plantar fasciitis is a condition causing heel pain. Supporting the arch, the plantar fascia, a thick band of tissue connecting the heel to the ball of the foot, can become inflamed or can tear. The condition develops when repeated weight-bearing activities put a strain on the plantar fascia. People who are diagnosed with plantar fasciitis also may have heel spurs, a bony growth that forms on the heel bone. However, people with heel spurs may not experience pain.
Plantar fasciitis occurs most frequently in people in their 40s but can occur in all age groups.
The condition can develop in athletes who run a great deal and in non-athletes who are on their feet most of the day, such as police officers, cashiers, or restaurant workers.
Signs and Symptoms
The onset of symptoms of plantar fasciitis frequently occurs with a sudden increase in activity. You might feel a stabbing pain on the underside of your heel, and a sensation of tightness and/or tenderness along your arch.
People with plantar fasciitis may experience pain:
- In the morning, when stepping out of bed and taking the first steps of the day
- With prolonged standing
- When standing up after sitting for awhile
- After an intense weight-bearing activity such as running
- When climbing stairs
- When walking barefoot or in shoes with poor support
As your body warms up, your pain may actually decrease during the day but then worsen again toward the end of the day because of extended walking. Severe symptoms may cause you to limp.
How Is It Diagnosed?
The physical therapist’s diagnosis is based on your health and activity history and a clinical evaluation. Your therapist also will take a medical history to make sure that you do not have other possible conditions that may be causing the pain. Sharing information about the relationship of your symptoms to your work and recreation, and reporting any lifestyle changes, will help the physical therapist diagnose your condition and tailor a treatment program for your specific needs.
To diagnose plantar fasciitis, your therapist may conduct the following physical tests to see if symptoms occur:
- Massaging and pressing on the heel area (palpation)
- Gently stretching the ankle to bend the top of the foot toward the leg (dorsiflexion)
- Gently pressing the toes toward the ankle
How Can a Physical Therapist Help?
Physical therapists are trained to evaluate and treat plantar fasciitis.
When you are diagnosed with plantar fasciitis, your physical therapist will work with you to develop a program to decrease your symptoms that may include:
- Stretching exercises to improve the flexibility of your ankle and the plantar fascia
- Use of a night splint to maintain correct ankle and toe positions
- Selection of supportive footwear and/or shoe inserts that minimize foot pronation and reduce stress to the plantar fascia
- Application of ice to decrease pain and inflammation
- Iontophoresis (a gentle way to deliver medication through the skin)
- Taping of the foot to provide short-term relief
Research shows that most cases of plantar fasciitis improve over time with these conservative treatments, and surgery is rarely required.
Can this Injury or Condition be Prevented?
Guidelines for the prevention or management of plantar fasciitis include:
- Choosing shoes with good arch support
- Replacing your shoes regularly, so that they offer arch support and provide shock absorption to your feet
- Using a thick mat if you must stand in one place for much of the day
- Applying good principles to your exercise program, such as including a warm-up and gradually building up the intensity and duration of your exercises to avoid straining the plantar fascia
- Stretching your calves and feet before and after running or walking
- Maintaining a healthy body weight
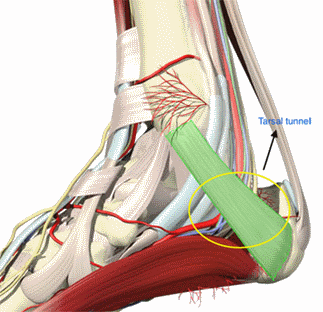
Tarsal tunnel syndrome (TTS) is a condition that develops when a nerve within the tarsal tunnel of the inner ankle is compressed. TTS can lead to alterations in sensation and movement of the foot, ankle, and lower leg, and/or pain. It is often associated with conditions causing increased compression or swelling in the lower leg. Physical therapists help people experiencing TTS to relieve their pain and restore their normal function.
What is Tarsal Tunnel Syndrome?
Often described as the carpal tunnel syndrome of the lower extremity, tarsal tunnel syndrome is a condition that results from the compression of the posterior tibial nerve as it runs through the tarsal tunnel (a structure made up of bone and tissue (retinaculum) on the inside of the ankle). As it passes through the tarsal tunnel, the tibial nerve divides into 3 branches that provide sensation for the heel and bottom of the foot, and aid in the foot's function. When this structure becomes compressed, symptoms, such as pain, numbness, and/or tingling may occur and radiate into the lower leg, foot, and toes. Individuals may also experience muscle weakness in the area.
How Does it Feel?
The most common symptoms of TTS result from irritation of the tibial nerve and its branches. People with TTS may experience:
- Pain, numbness, or tingling in the foot or ankle, which may radiate into the lower leg, foot, and toes
- Weakness in the muscles of the lower leg and foot
- Weakness of the big toe
- Foot swelling
- Symptoms that increase with prolonged standing or walking
- Symptoms that decrease with rest
- Altered temperatures of the foot and ankle
- Pain that disrupts sleep
How Is It Diagnosed?
There are several tests that can help a clinician determine if TTS is present. Your physical therapist and/or physician will first take a comprehensive health history, and inquire about your current symptoms. Then your physical therapist may conduct tests, such as:
- Gently tapping over the posterior tibial nerve in an attempt to reproduce your symptoms.
- Tensing of the posterior tibial nerve, a maneuver that looks and feels like a "stretch," in an attempt to reproduce your symptoms.
- Conducting a nerve condition study—a diagnostic test to determine the speed at which a nerve conducts information.
- Ruling out other conditions, such as plantarfasciitis (inflammation of the tissue that runs along the bottom of the foot).
How Can a Physical Therapist Help?
Physical therapists play a vital role in helping people experiencing TTS to improve and maintain their daily function and activities. Your physical therapist will work with you to develop a treatment plan to help address your specific needs and goals.
Because the signs and symptoms of TTS can vary, the approach to care will also vary. Your physical therapist may provide the following recommendations and care:
Nerve Gliding Activities. Gentle exercises that move and "glide" the nerves may help reduce symptoms and improve function.
Muscle Strengthening Exercises. Strengthening activities for any muscles affected by TTS, such as the tibialis posterior muscle in the back of your lower leg.
Balance and Coordination Activities. Work to improve your balance and coordination, which are often affected by TTS.
Orthotics/Taping/Bracing. Apply ankle taping, a custom orthotic, or bracing to position the foot to decrease stress on the posterior tibial nerve.
As with many conditions, education is key. Understanding the underlying mechanisms of TTS, and learning to recognize early signs and symptoms of stress may help you better manage the condition.
Can this Injury or Condition be Prevented?
Although there are no proven strategies for preventing TTS, there are ways to minimize stress to the foot and ankle, such as choosing appropriate footwear, wearing custom orthotics, minimizing the amount of time spent standing on hard surfaces, and improving and maintaining strength in the muscles of your legs, ankles, and feet. These strategies can be discussed further with your physical therapist.
In addition, early detection of the signs and symptoms of TTS will help you and your medical providers begin appropriate management of the condition, which may enhance your long-term well-being.
Peripheral neuropathy (PN) is a condition affecting the nerves of the body that results from nerve damage or disease. PN leads to alterations in sensation and movement and can cause pain. It also may be associated with other disease processes, such as diabetes. Although the symptoms of PN can cause discomfort and loss of function, there is evidence that PN may improve over time. Treatment by a physical therapist can help reduce symptoms and improve an individual's quality of life.
What is Peripheal Neuropathy?
PN is a condition that affects the nerves of your body. It is generally classified by the number of nerves affected, the type of nerve cells affected, or the process affecting the nerves.
Common classifications of PN include:
- Mononeuropathy. This is a condition only affecting 1 nerve. It is often a result of the compression of a nerve, which creates an onset of symptoms. Carpal tunnel syndrome is an example of a mononeuropathy, in which compression of the median nerve in the arm results in altered sensation, pain, and weakness.
- Polyneuropathy. This is a condition affecting many nerves and is generally a result of a disease process that affects the entire body, such as diabetes. This type of PN can result in an individual experiencing symptoms in various body parts, on both sides of the body.
It has been estimated that diabetic peripheral neuropathy affects approximately 12% to 50% of those with Type 2 diabetes. It has been predicted that 439 million people worldwide will develop diabetes by the year 2030, and 236 million will experience associated PN. - Neuritis: This is a condition that results from inflammation of a nerve. There are many causes of this type of PN, including infection, injury, or exposure to chemicals.
How Does it Feel?
To understand symptoms of PN, we must first understand that nerves have influence over 2 primary functions, and with PN, these functions may be altered: (1) sensation, and (2) movement.
People with PN may experience:
- Numbness and tingling, starting in the feet and hands, and eventually spreading up the limbs (in polyneuropathy).
- Loss or absence of sensation (the ability to sense contact with outside objects).
- Pain, often described as burning, sharp, or "electric-like."
- Increased sensitivity to light touch.
- Clumsiness or decreased coordination in the affected limb(s).
- Weakness or paralysis in the muscles or parts of the body affected by the nerve or nerves.
- Bowel or bladder changes (nerves controlling these functions may be affected).
- Temperature intolerances (generally to heat).
- Decreased ability to participate in normal functional activities.
How Is It Diagnosed?
A thorough examination by a medical professional will help determine if you have symptoms of PN. There are several methods and tests a clinician may use to make a diagnosis, such as testing your reflexes, sensation, and muscle strength.
If you have suspected symptoms, your physician may also order blood work, diagnostic imaging (such as MRI), or nerve conduction testing. These tests are generally ordered based on the suspected origin of symptoms.
How Can a Physical Therapist Help?
Physical therapists play a vital role in helping individuals improve and maintain functions that may be limited by PN. Your physical therapist will work with you to develop a treatment plan to help address your specific needs and goals.
Because the cause, type, and symptoms of PN can all vary, the approach to care will also vary. Your physical therapist may provide the following recommendations and care:
Nerve Gliding Activities. Your physical therapist can show you effective exercises that move and "glide" your nerves. Nerve gliding focuses on allowing the nerves to move more easily as you bend and straighten your joints. This therapy can help manage mononeuropathies.
Moderate-Intensity Exercise. Your physical therapist may recommend moderate-intensity exercises to help improve your strength and physical function.
Balance and Coordination Activities. Your physical therapist may work on strategies to improve your balance and coordination, both of which may be altered by PN. Improving balance and coordination can help decrease your risk of falling.
Education. Your physical therapist may educate you on how to safely manage PN. Your education will vary based on your individual needs, and may focus on improving your safety, preventing further complications, and finding alternative ways to perform certain tasks.
Can this Injury or Condition be Prevented?
Because there are many conditions associated with PN, such as diabetes, some basic lifestyle modifications can help reduce the risk of its development. PN currently affects approximately 3% to 4% of individuals over the age of 55 in the United States. That rate increases substantially in individuals with associated disorders, such as diabetes.
Maintaining an active, healthy lifestyle with routine checkups by your physical therapist, may help reduce your risk of developing certain types of PN and the complications associated with it. Your physical therapist is trained to notice any changes in factors, such as your strength, sensation, and functional ability that could suggest development of PN.
