-
 Injury keeping you out of the game?Our experts will get to the core of your fitness needs.OUR SERVICES
Injury keeping you out of the game?Our experts will get to the core of your fitness needs.OUR SERVICES -
 GET BACK TO THE ACTIVITIES YOU LOVEOUR SERVICES
GET BACK TO THE ACTIVITIES YOU LOVEOUR SERVICES -
 RESTORING YOUR PHYSICAL ABILITYOUR SERVICES
RESTORING YOUR PHYSICAL ABILITYOUR SERVICES -
 RESTORING YOUR QUALITY OF LIFEOUR SERVICES
RESTORING YOUR QUALITY OF LIFEOUR SERVICES -
 EVIDENCE BASED PRACTICEOUR SERVICES
EVIDENCE BASED PRACTICEOUR SERVICES -
 APPROPRIATE PROGRAM FOR A SUCCESSFUL RECOVERYOUR SERVICES
APPROPRIATE PROGRAM FOR A SUCCESSFUL RECOVERYOUR SERVICES -
 HELPING YOU ACHIEVE YOUR GOALSOUR SERVICES
HELPING YOU ACHIEVE YOUR GOALSOUR SERVICES
Back
If you have low back pain, you are not alone. At any given time, about 25% of people in the United States report having low back pain within the past 3 months. In most cases, low back pain is mild and disappears on its own. For some people, back pain can return or hang on, leading to a decrease in quality of life or even to disability.
If your low back pain is accompanied by the following symptoms, you should visit your local emergency department immediately:
- Loss of bowel or bladder control
- Numbness in the groin or inner thigh
These symptoms might indicate a condition called "cauda equina syndrome," in which nerves at the end of the spinal cord that control bowel and bladder function are being squeezed.
Although low back pain is rarely serious or life threatening, there are several conditions that may be related to your low back pain, such as:
- Degenerative disk disease
- Lumbar spinal stenosis
- Fractures
- Herniated disk
- Osteoarthritis
- Osteoporosis
- Tumors of the spine
While we used to believe the above list contributed directly to low back pain, research has shown these conditions are also present in people without any pain (asymptomatic).
Signs and Symptoms
The symptoms of low back pain vary a great deal. Your pain might be dull, burning, or sharp. You might feel it at a single point or over a broad area. It might be accompanied by muscle spasms or stiffness. Sometimes, it might spread into 1 or both legs.
There are 3 different types of low back pain:
- Acute – pain lasting less than 3 months
- Recurrent – acute symptoms come back
- Chronic – pain lasting longer than 3 months
Most people who have an episode of acute pain will have at least 1 recurrence. While the actual cause of low back pain isn't often known, symptoms usually resolve on their own. Psychosocial factors, such as self-confidence and a perceived ability to cope with disability; have been shown to be predictors of who might not recover from low back pain as expected. We used to believe the cause of low back pain was related directly to the tissues of our body, but are now understanding the condition to be more complex.
How Is It Diagnosed?
Your physical therapist will perform a thorough evaluation that includes:
- A review of your health history.
- Questions about your specific symptoms.
- A thorough examination that includes assessing the quality and quantity of your movements, and any movement behaviors that might put you at risk for delayed recovery.
- Tests to identify signs or symptoms that could indicate a serious health problem, such as broken bones or cancer.
- Assessment of how you use your body at work, at home, during sports, and at leisure.
For most cases of low back pain imaging tests, such as x-rays, computed tomography (CT) scans, and magnetic resonance imaging (MRI) are not helpful for recovery. For example, in a recently published article comparing patients who received an MRI first vs physical therapy first for low back pain, the patients who received an MRI first spent on average $4,793 more (with similar outcomes in each group). If your physical therapist suspects that your low back pain might be caused by a serious health condition, the therapist will refer you to other health care professionals for further evaluation.
How Can a Physical Therapist Help?
Your physical therapist can help you improve or restore mobility and reduce low back pain—in many cases, without expensive surgery or the side effects of medications.
If you are having low back pain right now:
- Stay active, and do as much of your normal routine as possible (bed rest for longer than a day can actually slow down your recovery.)
- If your pain lasts more than a few days or gets worse, schedule an appointment to see your physical therapist.
Not all low back pain is the same, so your treatment should be tailored to for your specific symptoms and condition. Once the examination is complete, your physical therapist will evaluate the results, identify the factors that have contributed to your specific back problem, and design an individualized treatment plan for your specific back problem. Treatments may include:
- Manual therapy, including spinal manipulation, to improve the mobility of joints and soft tissues
- Specific strengthening and flexibility exercises
- Education about how you can take better care of your back
- Training for proper lifting, bending, and sitting; for doing chores both at work and in the home; and for proper sleeping positions
- Assistance in creating a safe and effective physical activity program to improve your overall health
- Use of ice or heat treatments or electrical stimulation to help relieve pain
Can this Injury or Condition be Prevented?
As experts in restoring and improving mobility and movement in people’s lives, physical therapists play an important role not only in treating persistent or recurrent low back pain, but also in preventing it and reducing your risk of having it come back.
Physical therapists can teach you how to use the following strategies to prevent back pain:
- Use good body positioning at work, home, or during leisure activities.
- Keep the load close to your body during lifting.
- Ask for help before lifting heavy objects.
- Maintain a regular physical fitness regimen—staying active can help to prevent injuries.
There is evolving evidence suggesting that the best strategy in preventing disability and care-seeking for low back pain is simply understanding what we are learning about the topic of pain.
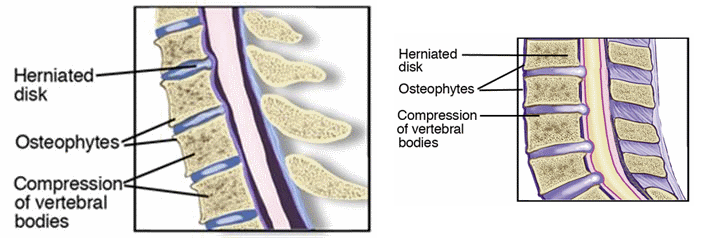
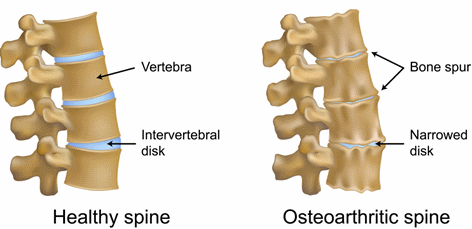
Your spine is made up of 33 vertebrae that are stacked on top of one another. Between each of these vertebrae is a rubbery piece of cartilage called an "intervertebral disk." (See images:Degenerative Disk Disease - Cervical | Lumbar) Imagine the disk as a tire, with gelatin filling the hole in the tire. The tire is called the "annulus," and the gelatin is called the "nucleus." When we're young—under 30 years of age—the disk is made mostly of gelatin. As we age, and sometimes with injury or excessive wear and tear, we start to lose some of that gelatin, and the volume of the disk decreases, resulting in less space between the vertebrae. The disk becomes flatter and less flexible, leaving less space between each set of vertebrae. Sometimes bone spurs form in response to this degeneration of the disk, making the spine stiff. When the rough surfaces of the vertebral joints rub together, pain and inflammation may result. Nerves may become irritated or compressed.
Disk degeneration might occur throughout several regions of the spine, or it might be limited to one disk. When it's part of the natural aging process, the degeneration does not always lead to pain. For some people, however, it can cause a great deal of pain and disability.
You are more likely to develop DDD if you:
- Smoke
- Are obese
- Do heavy physical work
- Don't get very much exercise
How Does it Feel?
You might have mild to intense neck and back pain—or no pain at all:
- A degenerative disk in the neck can cause pain in the arm, shoulder, or neck
- A degenerative disk in the low back might cause pain in the back, buttocks, or legs
The pain is often made worse by sitting, bending, and reaching. It may be worse first thing in the morning and after staying in any one position for a long time.
In severe cases, when DDD results in pressure on the nerves, it can lead to numbness, tingling, and even weakness in the arms or legs.
How Is It Diagnosed?
Your physical therapist will conduct a thorough evaluation that includes a review of your medical history and will use screening tools to determine the likelihood of DDD. For example, the therapist may:
- Ask you very specific questions about the location and behavior of your pain, weakness, and other symptoms
- Ask you to fill out a body diagram to indicate specific areas of pain, numbness, and tingling
- Perform tests of muscle strength and sensation to determine the severity of the pressure on your nerves
- Examine your posture and observe how you walk and perform other activities
- Measure the range of motion of your spine and your arms and legs
- Use manual therapy to evaluate the mobility of the joints and muscles in your spine
- Test the strength of important muscle groups
If you have muscle weakness and loss of sensation or very severe pain, special diagnostic tests, such as x-rays, may be needed. Physical therapists work closely with physicians and other health care providers to make certain that an accurate diagnosis is made and the appropriate treatment is provided.
Research shows that in all but the most extreme cases (usually involving muscle weakness or high levels of pain), conservative care, such as physical therapy, has better results than surgery.
After the evaluation, if your therapist suspects you have DDD and there are no major medical problems, treatment can begin right away.
How Can a Physical Therapist Help?
Your physical therapist's overall purpose is to help you continue to participate in your daily activities and life roles. The therapist will design a treatment program based on both the findings of the evaluation and your personal goals. The treatment program likely will be a combination of exercises.
Relieve Pain and Increase Movement
Your therapist will design:
- Stretching and flexibility exercises to improve mobility in the joints and muscles of your spine and your extremities—improving motion in a joint is often the key to pain relief
- Strengthening exercises—strong trunk muscles provide support for your spinal joints, and strong arm and leg muscles help take some of the workload off your spinal joints
- Aerobic exercise, which has been shown to be helpful in relieving pain, promoting a healthy body weight, and improving overall strength and mobility—all important factors in managing DDD
This might sound like a lot of exercise, but don't worry: research shows that the more exercise you can handle, the quicker you'll get rid of your pain and other symptoms.
Your physical therapist also might decide to use a combination of treatments:
- Manual therapy to improve the mobility of stiff joints and tight muscles that may be contributing to your symptoms
- Posture and movement education to show you how to make small changes in how you sit, stand, bend, and lift—even in how you sleep—to help relieve your pain and help you manage your condition on your own
- Special pain treatments—such as ice, electrical stimulation, or a short course of traction—for pain that is severe and not relieved by exercise or manual therapy
Once your pain is gone, it will be important for you to continue your new posture and movement habits to keep your back healthy.
Can this Injury or Condition be Prevented?
DDD usually is a natural result of aging. Research has not yet shown how to prevent it—but you can make choices that lessen its impact on your life and slow its progression. Many physical therapy clinics conduct regular educational seminars to help people in the community learn to take care of their backs and necks. These seminars often are free and provide demonstrations along with written information about exercises for the back and neck, instruction on proper lifting and sitting postures, and other tips to keep your back healthy.
Your physical therapist can help you develop a fitness program that takes into account your DDD. There are some exercises that are better than others for people with DDD, and your therapist will educate you about them. For instance:
- Exercising in water can often be a great way to stay physically active when other forms of exercise are painful.
- Exercises involving lots of twisting and bending need to be avoided in some individuals.
- Weight training exercises, though very important, need to be done with proper form to avoid stress to the back and neck.
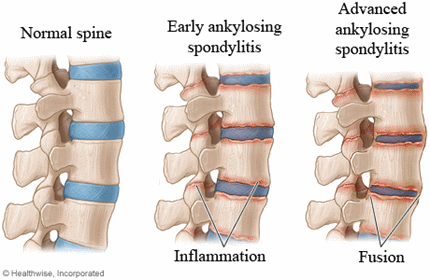
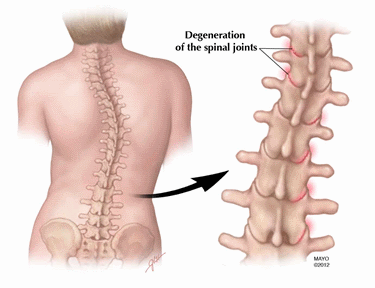
Ankylosing spondylitis (AS) is an inflammatory disease that causes pain and stiffness in the spine, pelvis, and other joints, like the hips, knees, feet, and shoulders. AS is a chronic (lifelong) disease, and it is hereditary. Although a majority of people who have AS carry a gene called HLA-B27, about 80% of people who have inherited the gene from a parent with AS do not develop the disease. The onset of AS is usually diagnosed in individuals between 17 and 45 years of age. Males are diagnosed 2 to 3 times more often than females, and tend to have more severe disease symptoms than females. Physical therapists help people with AS maintain productive lives by working with them to increase their strength, muscle flexibility, and joint mobility, and to improve their posture.
What is Ankylosing Spondylitis?
Ankylosing spondylitis (AS) is an inflammatory disease affecting the spine, pelvis, and joints throughout the body. AS causes abnormal bone growth, and causes joints to fuse (grow together) in the spine and in the sacroiliac joints (located between each hip and the pelvis). Vital organs like the heart, lungs, and eyes may also be affected. Rare complications include inflammation of the heart, scarring of the nerves of the spine, and kidney problems related to the long-term use of medication.
Although there is currently no cure for AS, proper treatment can help decrease the pain and stiffness associated with the disease. Medications decrease inflammation and localized swelling. If the hip joint becomes stiff and painful, total hip replacement may be performed.
How Does it Feel?
The first and most common symptom experienced with the onset of AS is pain in the sacroiliac joints and the low back. You may also gradually experience hip and shoulder pain. Pain is often accompanied by morning stiffness or stiffness after periods of prolonged inactivity, and usually improves after exercise or activity. Other common symptoms are fever, generalized fatigue, and loss of appetite.
Bony fusion or ankylosis typical of AS in the joints of the neck, spine, and hips causes progressive stiffness and can reduce your ability to turn your head, stand upright, or bend. AS can make maintaining good posture difficult, and can cause you to stoop forward. Poor posture makes it easier to lose your balance, and causes difficulty in walking, increasing the risk of falling. In advanced cases, osteoporosis (thinning of the bones) may occur, which increases the risk of fractures.
Inflammation is very common in AS. The inflammation usually is felt at the sites where ligaments and tendons attach to the bone. These sites are tender to touch and sometimes called “hot spots.” The heel and the back of the foot are common sites for tender spots, which can cause difficulty in standing and walking.
People with AS may develop difficulty breathing because the lungs and the joints where the ribs and spine attach become stiff, limiting chest expansion and causing shortness of breath, and increasing the risk of chest infections.
AS can also affect the soft tissues of the eye (in about 40% of cases), resulting in swelling in the eye (uveitis). Individuals may also experience eye redness, pain, "floaters," and an increased sensitivity to light.
How Is It Diagnosed?
If you see your physical therapist first for symptoms, such as chronic back pain, the physical therapist will take your medical history, and ask you to describe how your symptoms occurred, what symptoms you experienced first, and if they get worse with inactivity and better with activity.
Your physical therapist will perform a thorough evaluation of your posture, and the range of motion (movement) of your spine, hips, knees, and shoulders. Your physical therapist will also check to see if you have any tender spots around your spine, hips, and sacroiliac joints, and gently assess your ability to bend forward, bend backward, squat, and walk.
When your physical therapist suspects AS, your physical therapist will also measure your chest expansion when you take a deep breath and exhale. That will indicate how the AS may be affecting your rib joints and breathing function.
Your physical therapist will also observe your ability to walk and how you move from sitting to standing, and test your balance to determine if you have a fall risk.
If your physical therapist suspects AS, the physical therapist will consult with your physician for further tests, such as an X-ray or MRI of the spine and sacroiliac joints. Blood tests and genetic testing may also be recommended; a blood test positive for the HLA-B27 gene can indicate a risk of developing AS.
How Can a Physical Therapist Help?
Physical therapy will help improve your posture and joint mobility, reduce pain, and help you perform your everyday functional activities more easily. Your physical therapist may teach you:
Posture Training to improve your posture and help you avoid slouching or forward bending. This training is important to ensure that you maintain an upright posture.
Strengthening Exercises to strengthen your back and abdominal muscles and help you maintain proper posture and walking, and perform your activities of daily living.
Flexibility Exercises to maintain and improve joint mobility. Exercises for your leg and chest muscles, and gentle range-of-motion exercises help keep the spine and other joints from getting stiff. Aquatic exercises have been shown to decrease joint pain and improve movement in patients with AS.
Stretching Exercises for the trunk muscles to improve chest expansion.
Deep-Breathing Exercises to improve chest expansion and help you breathe better. Improved breathing increases oxygen and blood flow in the body, which can help decrease stiffness, pain, and fatigue.
Pain Management Techniques, such as using ice or heat packs to manage inflammation and pain in the joints. Your physical therapist may prescribe a TENS unit, which is an electrical stimulation treatment used to alleviate pain.
Individual Activities to improve your functional ability and energy, and help reduce fatigue. Your physical therapist will teach you how to move your body efficiently when performing daily activities to avoid strain. Your physical therapist may recommend using an assistive device, such as a cane or walker to improve your walking, lessen pain, and lower your risk of falling.
Your physical therapist will partner with you to ensure that you maintain your best posture, flexibility, joint mobility, and muscle strength, so you can lead a productive, fulfilling life. We are here to help!
After Surgery
If your hip joints have developed severe arthritis, your physician may recommend a total hip replacement. Your physical therapist will help you improve your walking, your joint range of motion, and your leg strength following surgery, so you can safely return to your usual daily activities.
Can this Injury or Condition be Prevented?
As it is an inherited disease and it cannot be prevented. However, functional limitations may be reduced or prevented by participating daily in a program of posture correction, stretching, and strengthening exercises
What is Osteoarthritis of the Spine?
As we age, the discs in our spine can wear, begin to bulge, and become narrowed. These changes can put strain on the cartilage, ligaments, and joints at the involved level of the spine and may cause pain. The narrowing of the disc also results in narrowing of the space between the spinal joints, called the "facet" joints. Weight-bearing forces on the joints increase because of these disc changes. As a result, the cartilage covering the joint surface can begin to fray and wear away over time. If your cartilage wears down so that your bones begin to rub together, it can result in enlarged joints, inflammation, stiffness, and pain.
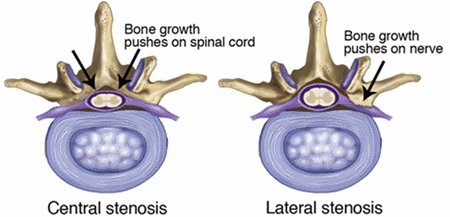
As OA of the spine progresses, your body will try to repair it by growing new bone. This bony growth is called a "bone spur." Spur development can result in a condition known as spinal stenosis. Most often this disorder affects men and women over 50 years of age. If the spurs enlarge, they can create a narrowing of the spaces in the spine. The narrowing can involve small or large areas and can result in pressure on nerves near the involved joints, resulting in symptoms that may include pain, tingling, numbness, or burning.
Osteoarthritis (OA) of the spine is a condition that usually occurs with aging and is typically diagnosed after age 50. Its causes include injury to the spine, wear and tear on the discs of the spine (often associated with obesity), or an inherited tendency to develop OA. Sometimes the cause is unknown. OA of the spine may cause pain and stiffness; and make it difficult to bend over, perform weight-bearing activities such as walking, and accomplish daily tasks such as dressing and bathing. Your physical therapist will help you manage your condition, lessen your discomfort, and get moving again.
How Does it Feel?
Symptoms of OA of the spine vary from person to person and can range from mild to disabling. You may not have symptoms even though the condition is present. Its onset and progression can be quite slow.
With early or mild disease, symptoms will be intermittent, or come and go. You might feel stiffness or aching after sitting a long time, on waking in the morning, or after vigorous activity. You or your family may notice changes in your posture. Some people will bend forward or shift to the side. With more advanced OA of the spine, symptoms will become more constant and tend to interfere more with your daily activity, especially with walking and standing.
Common symptoms of OA of the spine include:
- Pain in the back or neck
- Pain that is worse after prolonged inactivity, on getting up in the morning, or after physical activity
- Pain that worsens with standing and walking, and gets better with sitting or lying down
- Stiffness after prolonged inactivity, on getting up in the morning, or with movement of the involved area of the spine
- With a more advanced condition, symptoms that do not improve with rest and that interfere with sleep
- Pain, burning, or tingling sensations that spread to the shoulder or arm, or to the buttocks or leg
- Difficulty performing normal daily activities, such as dressing and bathing, as well as walking and standing as the condition progresses
- Pain caused by the weakening of muscles surrounding the joint, due to inactivity
How Is It Diagnosed?
Your physical therapist will perform a thorough evaluation and may:
- Ask specific questions about your past and current health and use of medication
- Have you complete a questionnaire about how you are functioning in your daily life
- Ask how your symptoms came about, how long you have had them, where they are located, how and when the pain occurs, and other questions, to form a clear picture of your individual situation
Your physical therapist will then conduct a physical examination and may:
- Evaluate your posture and spinal alignment, and measure the range of motion and flexibility of your spine and the extremities (arms or legs) in the involved area
- Check your nerve function with reflex, sensation, and strength testing
- Observe how you use your body for home, work, and social/leisure activities
- Check your balance to determine your risk of falling
The information learned in your evaluation will help your physical therapist prescribe a program to ease your discomfort, boost your quality of life, and get you moving your best.
Imaging tests such as x-rays, computed tomography (CT) scans, and magnetic resonance imaging (MRI) may be requested but are not necessary in every case. However, if your physical therapist suspects that your pain might be caused by an underlying condition, he or she may request testing from your physician and/or refer you to your physician for further evaluation. Your physical therapist will work with your physician to provide the best diagnosis and treatment.
How Can a Physical Therapist Help?
Your physical therapist will help you set goals to reduce your symptoms and slow the progression of the disease. You'll learn how to safely exercise and continue to participate in your normal daily activities.
Your physical therapist can help with a variety of treatment options, including:
- Exercise: Exercise is the most important treatment to lessen your pain and improve your mobility. Your physical therapist will prescribe specific low-impact activities that will strengthen your spine, abdomen, and hip muscles—to improve your ability to stand, walk, and balance, and lower your risk of falling.
Caution: Please consult your physical therapist or doctor before starting any exercise program.
- Stretching: Your physical therapist will prescribe specific stretching exercises for your spine, arms, or legs based on the results of your initial evaluation. Obese individuals are in special need of stretching and exercises. Combined with strengthening, stretching may help slow the progression of the disease.
- Symptom management: Symptom management means learning to feel better and remain active. Sometimes people are fearful that increased activity will worsen their symptoms or increase their pain. Your physical therapist will help you learn how to be more active without worsening your symptoms. He or she will help you find your appropriate activity levels, and develop a unique program to keep you moving.
- Daily activity training: Your physical therapist can teach you how to get in and out of bed, in and out of the bathtub, or out of a chair, and how to bend and walk with more ease.
- Use of modalities: Treatment "modalities" such as heat or ice may be used to help manage your symptoms.
- Manual therapy: Your physical therapist may use gentle hands-on techniques (manual therapy) to help improve your spinal flexibility and ease stiffness.
- Balance and walking training: Exercises and instruction may be used to improve your balance safely,and reduce your risk of falls.
- Specialized braces or taping: Your physical therapist may use taping or specialized braces to help support your joints. Back bracing is used most in more advanced conditions.
- Weight control: If you are obese, you are likely to have more spinal impairment in your upper back. Your physical therapist can help you improve your activity levels, and refer you to nutritional experts.
Remember, all cases of OA of the spine are different. Your physical therapist will choose the best treatment options for you based on his or her evaluation of your specific problem.
Following Surgery
The predominant treatment for OA of the spine is non-surgical. However, symptoms that interfere with bowel or bladder function and cause problems with the nervous system may require surgery.
Immediately after surgery, a physical therapist will visit you in the hospital to help you get out of bed and walk, and possibly use a cane or walker for safety. When adequate healing has occurred, you may be sent for outpatient physical therapy to continue to improve your walking, and to progress your exercise program.
Can this Injury or Condition be Prevented?
OA occurs as you age, but is not a direct result of getting older. There are many factors that put you at risk of developing OA, including your family history. Other factors include previous injury, heavy use of your spine over a period of time, and obesity.
If you are obese, you have a higher likelihood of having OA in the spine. Weight loss is important to lower joint stress, and possibly prevent the onset of OA. If you already have OA, weight loss may prevent worsening of the condition. Exercise and increasing your physical function along with dietary modifications can also decrease your pain.
Prevention of injuries, especially sports injuries, may prevent the onset of OA. It is important to perform your physical activities or exercises to the point of fatigue, but not to force yourself beyond that point. Regular conditioning and strengthening exercises will improve the ability of your muscles to work, easing the stress on your joints.
Sacroiliac joint (SIJ) dysfunction is a lower back/pelvic condition that can result from joint stiffness (hypomobility) or slackness (hypermobility) at the sacroiliac joints in the pelvis. The condition can affect both men and women of all ages, but is more common in females. Symptoms typically are present on 1 side of the back, and affect 10% to 25% of patients with complaints of low back pain. Physical therapists design individualized treatment programs to address SIJ dysfunction based on the specific cause of each person's condition, and treatment goals.
What is Sacroiliac Joint Dysfunction?
The sacroiliac joint is a joint between the sacrum and the ilium, or pelvic bone. The 2 sides of the sacroiliac joint normally work together. If 1 side becomes stiff, they will not move together and this causes pain or muscle stiffness in the area. Pain is often made worse with walking and bending activities. It is also possible that 1 side may become too loose (lax) as well, resulting in SIJ dysfunction. This may occur during the menstrual cycle or pregnancy due to hormonal changes that cause the ligaments to become more lax.
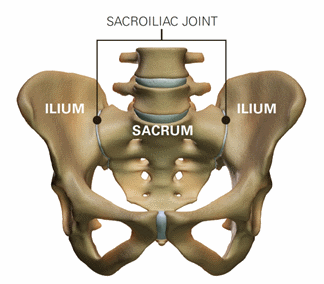
SIJ dysfunction can occur with injury, such as when a person falls and lands on 1 side of the body and alters the position of the joint, or when an athlete overtrains. Muscle imbalances and hip problems, such as hypermobility or dysplasia, may also lead to SIJ dysfunction. Sacroiliac pain is also related to some types of arthritis, such as ankylosingspondylitis, an inflammatory process most often affecting the lower back, which may cause the vertebrae to fuse.
How Does it Feel?
People with SIJ dysfunction may experience:
- Pain that may be sharp, stabbing or dull, localized to 1 side of the pelvis/low back, groin, or tailbone.
- Pain that may radiate down to the knee.
- Pain with movements, such as standing up from a sitting position, turning in bed, or bending/twisting.
- Muscle tightness and tenderness in the hip/buttock region.
- Pain with walking, standing, and prolonged sitting.
- Pain that is worse when standing and walking, and eases when sitting or lying down.
How Is It Diagnosed?
When you see your physical therapist, the therapist will ask you questions about your current condition, such as:
- When did the pain start?
- What happened to cause the pain to start?
- Did you experience a fall or injury?
- Have you experienced similar symptoms in the past?
- Where is the pain located?
- What specific movements/activities cause your pain?
- Are you pregnant, or have you recently given birth?
Your physical therapist will then conduct a physical evaluation. Your therapist may examine the position of your spine, conduct strength tests of the hip, pelvic, and lower extremity muscles, and gently perform movement tests to assess your mobility and flexibility. Specialized tests will be performed to rule out any problems that may require other medical intervention. If further medical intervention is required, your physical therapist may refer you to a physician who specializes in SIJ dysfunction or other conditions that may be causing your symptoms.
Once SIJ dysfunction has been confirmed, your physical therapist will work with you to determine your personalized treatment program.
How Can a Physical Therapist Help?
Your physical therapist will design a targeted treatment program based on your evaluation and your goals for a safe return to sport or daily activities. Treatment may include:
- Manual therapy. Often, manual therapy for SIJ dysfunction includes soft tissue release or massage for tight and sore muscle groups. Manual therapy and muscle energy techniques (MET) are used to correct pelvic/SIJ alignment. MET uses your own muscle contractions to realign the position of the pelvis, and can be a source of pain relief. Joint mobilizations/manual therapy uses gentle movements to improve mobility of the hip, SIJ, and low back.
- Flexibility exercises. Stretching exercises may be prescribed to improve the flexibility of tight muscles. They may also help to improve movement in the spine and lower extremities, and help decrease stress at the sacroiliac joint during daily activities.
- Strengthening exercises. Strengthening helps to improve the stability of the sacroiliac and spinal joints, which helps to reduce ligament strain and pain. These exercises are focused on weak muscles, including the lower abdominal, pelvic floor, and buttocks muscles.
- Body mechanics. How you move and use your body for daily work and other activities can contribute to your SIJ dysfunction and pain. Your physical therapist will teach you how to improve your movements or body mechanics based on your specific daily activities. The physical therapist may also make recommendations to improve activities, such as sitting, or lifting and carrying objects.
- Modalities. Hot and cold treatments are often prescribed to loosen up tight muscles prior to treatment, or to alleviate pain following exercise. Electrical stimulation uses electricity to target nerve fibers that send pain signals to the brain, and may also be used in conjunction with ice to provide pain relief.
- Braces. Your physical therapist may also recommend wearing a sacroiliac belt, designed to provide support to the sacroiliac joints. It is used to provide stability during daily activities as your strength returns, and flexibility improves. This modality is especially helpful for pregnant women.
All treatments prescribed by the physical therapist will be based on your specific case.
Can this Injury or Condition be Prevented?
Fall prevention, the use of proper body mechanics (such as correcting your posture), and maintaining healthy activity levels are all ways that SIJ dysfunction may be prevented. Adhering to appropriate strength and flexibility programs can maintain muscle mobility and strength to keep the area stable when joint hypermobility is present. Your physical therapist can work with you to strengthen and stretch your joints and muscles to prevent conditions like SIJ dysfunction from occurring.
To prevent a recurrence of SIJ dysfunction after physical therapy treatment is completed, you will need to continue performing your home-exercise program. It is imperative that you do this to maintain your strength and flexibility. Improving and maintaining muscle strength will continue to provide stability for the sacroiliac joint and low-back ligaments after an injury.
What is Scoliosis?
Scoliosis is a condition that affects the normal shape of the spine, altering a person's overall trunk alignment and posture. Scoliosis causes the spine to move to the side and turn. This condition can occur at any time during the lifespan, but is more commonly detected during adolescence. Scoliosis affects 2% to 3% of the general population, and is more common in females than males. Scoliosis ranges from mild to severe cases, requiring a variety of treatments. The more severe cases may require surgery. Scoliosis is best managed with a team approach that includes the family, orthopedic physician or surgeon, orthotist, and physical therapist.
The Scoliosis Research Society defines scoliosis as a curvature of the spine to the side that also includes rotation. As previously mentioned, scoliosis causes postural and trunk alignment changes that cannot be corrected by “standing up straight. On an x-ray, the spine may appear to have an "s" or "c" shape. The severity of scoliosis is determined by measuring the angle of the curvature, also called a Cobb angle. A minimum of "10° of Cobb" needs to be present for a diagnosis of scoliosis.
Adolescent idiopathic scoliosis (AIS), the most common type of scoliosis, is diagnosed in children aged 10-18 years. Idiopathic means no identifiable cause is known, but 30% of children with AIS have some family history of the condition.
Other types of scoliosis include congenital, neuromuscular, and early onset (infantile and juvenile).
- Congenital scoliosis is caused by a deformity in the bones of the spine that occurs during a baby's early development in the womb.
- Neuromuscular scoliosis is caused by a medical condition of the nervous system, such as cerebral palsy or muscular dystrophy, which triggers weakening of the muscles that support the spine.
- The cause of early onset scoliosis is not known. Early onset scoliosis includes infantile scoliosis diagnosed from birth to 3 years of age, and juvenile scoliosis diagnosed before the age of 10.
How Does it Feel?
Scoliosis is usually a pain-free condition, but pain may occur as the spine curves abnormally and affects the surrounding muscles and joints. These changes may alter a person's alignment, posture, and movement patterns, causing irritation and pain. Muscles that usually support the spine may become imbalanced in scoliosis, leading to a loss of strength and flexibility. A person with scoliosis may note:
- Uneven shoulder height.
- Uneven hip height.
- An uneven waistline.
- A general sense that the 2 sides of the body don't line up.
- Pain in the areas surrounding the spine, including the shoulder, pelvis, and hip.
- Pain with specific movement or activity.
A primary goal of physical therapy is to identify conditions, such as scoliosis, help the individual restore and maintain mobility so they can function at their personal best, and improve their quality of life.
How Is It Diagnosed?
Scoliosis is usually detected during a physical examination or school screening performed by a pediatrician, school nurse, or physical therapist, with the goal of early detection and treatment.
An initial visit with a physical therapist includes a thorough medical history, and specific questions about the family health history and current activities. Your physical therapist will closely examine the spine in several positions and check factors, such as strength and flexibility, and any feelings of tenderness or swelling. You or your child may be asked to briefly demonstrate the activities or positions that cause difficulty or pain.
The physical therapist also will identify symptoms the individual is experiencing that are caused by the curve to the spine. If the patient goes to the physical therapist before seeing a physician, the individual will be referred to an orthopedic physician, since a radiograph is needed to confirm a diagnosis of scoliosis.
How Can a Physical Therapist Help?
The variety of treatment options for scoliosis includes physical therapy, bracing, and surgery. Determining the best course of treatment is based on the type and severity of the scoliosis, the patient’s age, and the guidelines established by the Scoliosis Research Society.
Physical therapists can provide care during any of the phases of scoliosis treatment, including bracing or postsurgery. They will evaluate and assess the posture and movement patterns of the whole body, noting any limitations caused by changes in the spine, and address other symptoms, such as pain and muscle imbalances.
Your physical therapist will work with you and your child to develop an individualized plan tailored to the type and severity of the scoliosis as well as patient goals. Your physician will continue to closely monitor progress throughout the course of rehabilitation.
Physical therapy treatments may include:
Range-of-Motion Exercises. Your physical therapist will design a gentle range of motion treatment program to prevent limitations or to increase the body's range of motion, if movement limitations are present.
Strength Training. Your physical therapist will design a treatment program to strengthen any muscles surrounding the spine or in other parts of the body that have been weakened by the change in the spine’s position, such as the hips, shoulders, or even the head and feet.
Manual Therapy. Physical therapists are trained to gently restore motion to joints and muscle tissue that may have become restricted due to scoliosis. They may use their hands to help guide and retrain movement patterns.
Modalities. Several additional treatments, such as ice, heat, electrical stimulation or ultrasound may aid in achieving physical therapy goals. Your physical therapist will choose the most appropriate modalities for your particular case.
Functional Training. Physical therapists are trained to be experts in assessing movement patterns, providing education on proper movement patterns, and retraining the body for optimal movement.
Education. Your physical therapist will provide information about scoliosis and the effects on the body and movement.
Can this Injury or Condition be Prevented?
Scoliosis cannot be prevented. Research is ongoing regarding treatments to stop the progression of scoliosis, such as bracing. A recent study has demonstrated that bracing is effective at limiting the progression of spinal curves. The primary goals of physical therapy are to manage symptoms and maximize each individual's functional capacity. A team approach to treating scoliosis works best.
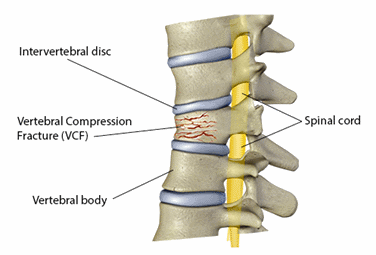
What are Spinal Compression Fractures?
The entire spine is made up of 24 bones, called vertebrae. There are 7 cervical vertebrae, 12 thoracic vertebrae, and 5 lumbar vertebrae. Compression fractures occur most commonly in the middle back or thoracic spine in the T10, T11, and T12 areas, and in the lower back or lumbar spine at the L1 area.
A fracture in the spine occurs when the vertebrae or small bones that form the spine collapse or break. There are 5 different types of spinal fractures, but the most common type is the spinal compression fracture. A compression fracture occurs when the vertebrae collapse together. These fractures commonly occur in people with osteoporosis, women over the age of 50 who are postmenopausal, or any individuals over the age of 60 who may have weakened bones. Spinal compression fractures can also occur when cancer affects the spine. Approximately 700,000 cases of spinal compression fractures per year occur in the United States due to osteoporosis. It is estimated that 25% of women who are postmenopausal in the United States have had a vertebral compression fracture due to weakening of the bones from changes in hormones that occurred during this period of their lives. Physical therapists help patients with spinal compression fractures reduce their pain and improve their strength, flexibility, and overall function.
When the spinal bones are weakened, a simple activity, such as bending to lift an object, twisting, or even coughing, laughing, or sneezing can cause a spinal compression fracture. These small compression fractures can gradually cause the spine to become shorter and less stable, and can weaken the entire spine. Generally the compression fractures cause the bone to break down in the front (anterior) portion of a vertebra, while the back (posterior) portion of the vertebra remains solid. This frontal breakdown causes the spine to round forward, which is called a Dowagers Hump or thoracic kyphosis.
A spinal compression fracture may also be caused by trauma to the spine, such as a car accident, hard fall, or blow to the head. Physical therapy begins after the compression fracture has been deemed "stable," which can take up to 8-10 weeks. Physical therapists help people with spinal compression fractures reduce their back pain and improve their flexibility, strength, and overall function, and restore the activity levels they had prior to the injury. Physical therapy will also help patients reduce falls risk that can lead to future fractures.
How Does it Feel?
The symptoms of a spinal compression fracture are often overlooked as regular back pain that occurs with aging or a muscle strain. Approximately two-thirds of nontraumatic compression fractures of the spine go untreated. If you are experiencing a spinal compression fracture, you may feel:
- Back pain that may be sudden or may worsen over time
- Pain, numbness, or paralysis that occurs in the legs (eg, traumatic compression fracture, as small pieces of bone can lodge into the spinal cord)
- Back pain that worsens with upright postures, such as standing and walking
- Pain felt with coughing, sneezing, laughing, or breathing deeply
- Back pain that relieves with lying down
- Pain and difficulty with bending or twisting
- Tenderness over a specific region of the spine
- A stooped-over posture called a Dowagers Hump or thoracic kyphosis
- Loss of overall height, possibly as much as 6 inches
- In cases where the spinal cord is compressed: numbness, tingling, difficulty walking, loss of bowel and/or bladder control
Several diagnostic tests may be ordered by a physician to determine if a spinal compression fracture has occurred. They may include:
- Spinal x-rays
- Bone density testing to measure the thickness of the bone
- CT scan or MRI imagery (in severe traumatic cases)
How Can a Physical Therapist Help?
Your physical therapist will perform a complete evaluation, including your past medical history, any medications you may be taking, and your current symptoms. Your regular activities of daily living will be discussed so your physical therapist can design a treatment plan specific to your personal needs and goals.
Your physical therapist will perform a physical examination of your spine. The therapist will touch areas of your spine to determine any pain or tenderness of the spinal areas involved. Your spinal movements (range of motion) will be assessed in your neck (cervical spine), middle back (thoracic spine), and lower back (lumbar spine). Your physical therapist will also measure the strength in your spine, legs, and shoulders. Balance testing will be performed to determine if you are at risk for falls that can lead to other fractures.
Surgery is rarely needed in cases of compression fracture. It may take 8 to 10 weeks after your diagnosis for the spinal compression fracture to heal. During the healing process, you may take pain medication and medications to improve your bone density, as determined by your physician. Your physician may choose to have you wear a back brace for extra support. Braces are used with caution, as they can contribute to muscle weakness. You will also need to reduce your overall activity level during this time to allow the bones to heal. This means no heavy lifting, bending, or twisting activities, and may require a short period of bed rest, depending on the severity of the fracture.
After your spinal fracture is healed and it is considered safe to increase your activity level without risk of reinjuring the bone, you may see a physical therapist for an evaluation to begin treatment. During the healing process when your mobility is limited, muscles in the core, hips, and back can become weakened. This weakness can make it difficult to resume your regular activities, and the weakness can put you at greater risk for falls.
Your physical therapist can help you regain the strength and mobility that you may have lost while the fracture healed. Your treatment plan may include:
Pain Management. In the initial recovery phase, the goal of physical therapy will be to reduce any pain and inflammation in the affected area. Manual therapy, including soft tissue mobilizations and gentle massage, may help manage your pain as well as the application of ice and electrical stimulation. After the fracture has healed, moist heat can help decrease pain due to muscle spasms in the spinal region.
Flexibility Exercises. You may learn and perform gentle spinal range-of-motion exercises for the neck, thoracic, lumbar, hip, and shoulder areas.
Strengthening Exercises. Bones strengthen when forces are applied to them. Your physical therapist will prescribe gentle weight-bearing exercises to help stimulate your bone strength. Upper- and lower-body as well as abdominal and back muscle-strengthening activities will be performed, including the use of light weights.
Posture and Movement Education. Your physical therapist will teach you how to maintain safe postures and spinal positions to protect the vertebrae from undue stress. For instance, you will learn safe positions for sleeping, sitting, and standing. You will also learn proper body mechanics for performing tasks at home, such as bending and lifting. Your physical therapist will also design an individualized home-exercise program, which you can continue after you have completed your physical therapy program.
Fall Prevention. Your physical therapist will teach you exercises to improve your balance and steady your walking gait to prevent falls. You may perform gentle exercises on a variety of surfaces. You will also learn ways to modify your home environment to make it safer and reduce the risk of a fall.
Referral to a Nutritionist. You may be referred to a nutritionist for a consultation. Getting the proper nutrients from your diet can help improve bone growth and strength.
Can this Injury or Condition be Prevented?
There are several ways in which a spinal compression fracture can be prevented. Physical therapists recommend that you:
- Eat a well-balanced diet to promote bone health.
- Stop smoking.
- Keep alcohol consumption moderate.
- Take calcium and vitamin D supplements as recommended by your physician.
- Exercise regularly, including weight-bearing activities, such as walking and using light weights.
- Reduce fall risk with home modifications and balance exercises as recommended by your physical therapist.
- Maintain proper posture and body mechanics when performing activities of daily living.
What Is Spinal Stenosis?
It's estimated that as many as 75% of us will have some form of back or neck pain at some point in our lifetime. The good news is that most of us will recover without the need for surgery—and conservative care such as physical therapy usually gets better results than surgery. Spinal stenosis is one cause of back and neck pain. It affects your vertebrae (the bones of your back), narrowing the openings within those bones where the spinal cord and nerves pass through.
Spinal stenosis is a narrowing within the vertebrae of the spinal column that results in too much pressure on the spinal cord (central stenosis) or nerves (lateral stenosis). Spinal stenosis may occur in the neck or in the low back.
The most common causes of spinal stenosis are related to the aging process in the spine:
- Osteoarthritis is a deterioration of the cartilage between joints. In response to this damage, the body often forms additional bone (called "bone spurs") to try to support the area. These bone spurs might cause pressure on the nerves as they exit the spinal canal.
- Normal aging and wear and tear can result in a flattening of the disks that provide space between each set of vertebrae. This narrowed space allows less room for the nerve to exit from the spinal cord, and sometimes pieces of disk material cause pressure on the nerves.
Spinal injuries, diseases of the bone (such as Paget disease), spinal tumors, and thickening of certain spinal ligaments also may lead to spinal stenosis.
In most cases, symptoms of spinal stenosis can be effectively managed with physical therapy and other conservative treatments. Only the most severe cases of spinal stenosis need surgery or more aggressive treatments.
Signs and Symptoms
Spinal stenosis may result in such symptoms as:
- Pain, numbness, tingling, or weakness in your arms and shoulders, legs, or trunk
- Occasionally, problems with bowel or bladder function
If you have spinal stenosis in the neck, you may have weakness, numbness, and pain in the arms and often in the legs, depending on which nerves are affected. You might not have any pain in the neck itself.
If you have spinal stenosis in the low back (lumbar spinal stenosis), you might have pain, numbness, and weakness in the low back and legs, but not in the arms. Your symptoms might get worse with walking and improve with sitting.
How Is It Diagnosed?
Because the symptoms of spinal stenosis are often similar to those of other age-related conditions, a careful diagnosis is important. Your physical therapist will conduct a thorough evaluation, including a review of your medical history, and will use screening tools to determine the likelihood of spinal stenosis. The therapist may:
- Ask you very specific questions about the location and nature of your pain, weakness, and other symptoms
- Ask you to fill out a body diagram to indicate specific areas of pain, numbness, and tingling
- Perform tests of muscle strength and sensation to determine the severity of the pressure on your nerves
- Examine your posture and observe how you walk and perform other activities
- Measure the range of motion of your spine and your arms and legs
- Use manual therapy to evaluate the mobility of the joints and muscles in your spine
- Test the strength of important muscle groups
If you have muscle weakness and loss of sensation or very severe pain, special diagnostic tests, such as x-rays, may be needed. Physical therapists work closely with physicians and other health care providers to make certain that an accurate diagnosis is made and the appropriate treatment is provided.
Research shows that in all but the most extreme cases (usually involving muscle weakness or high levels of pain), conservative care, such as physical therapy, has better results than surgery.
How Can a Physical Therapist Help?
Your physical therapist's overall purpose is to help you continue to participate in your daily activities and life roles. The therapist will design a treatment program based on both the findings of the evaluation and your personal goals. The treatment program likely will be a combination of exercises.
Relieve Pain and Increase Movement
Your therapist will design:
- Special exercises to take pressure off the nerves to relieve pain
- Stretching and flexibility exercises to improve mobility in the joints and muscles of your spine and your extremities—improving motion in a joint is often the key to pain relief
- Strengthening exercises—strong trunk muscles provide support for your spinal joints, and strong arm and leg muscles help take some of the workload off your spinal joints
- Aerobic exercise to increase tolerance for activities such as walking that might have been affected by the spinal stenosis
This might sound like a lot of exercise, but don't worry: research shows that the more exercise you can handle, the quicker you'll get rid of your pain and other symptoms.
Your physical therapist also might decide to use a combination of treatments:
- Manual therapy to improve the mobility of stiff joints that may be contributing to your symptoms
- A special harness-type device attached to a treadmill that helps to reduce pressure on the spinal nerves during walking
- Posture education to help you learn to relieve pressure on the nerves by making simple changes in how you stand, walk, and sit
- Special pain treatments, such as ice or electrical stimulation, for pain that is severe and not relieved by exercise or manual therapy
Can this Injury or Condition be Prevented?
Spinal stenosis usually is a natural result of aging. Research has not yet shown us a way to prevent it. However, we do know that you can make choices that lessen the impact of spinal stenosis on your life and even slow its progression:
- Regular exercise strengthens the muscles that support your back, keeps the spinal joints flexible, and helps maintain a healthy body weight. All of these factors help reduce the wear and tear on the spine.
- Using supportive chairs and mattresses and avoiding activities that can lead to injury—such as heavy lifting—can help protect your back.
Your physical therapist can help you develop a fitness program that takes into account your spinal stenosis. There are some exercises that are better than others for people with spinal stenosis, and your therapist can educate you about what you should avoid. For instance, because walking is usually more painful than sitting, bicycling may be a better way for you to get regular physical activity. Trunk strengthening exercises often need to be modified to avoid movements such as backward bending that might cause extra pressure on the nerves.
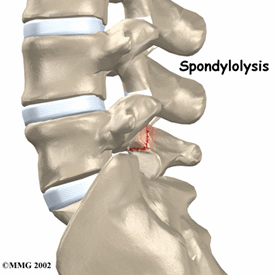
Spondylolysis (spon-dee-low-lye-sis) is a stress fracture of a section of the lumbar spine; most frequently the fifth vertebrae. The injury can occur on the left, the right, or both sides of the vertebrae. Spondylolysis occurs in up to 11.5% of the general population in the United States, and is most frequently seen in young males. Spondylolysis is a common cause of low back pain experienced in late childhood and adolescence. Highly active teens, both boys and girls who engage in activities that require lifting heavy loads, repeated backward bending of the back, or twisting of the trunk, are most at risk for spondylolysis, including athletes participating in activities like football, hockey, gymnastics, or dance. Only a small percentage of cases of spondylolysis require surgery, and 85% to 90% of young patients recover in 3 to 6 months with proper treatment.
Spondylolisthesis (spon-dee-low-lis-thee-sis) describes the forward slippage of a vertebrae over the vertebrae beneath it. Because the mechanism of injury, age of the patient, symptoms, and treatment are similar for both conditions, spondylolysis and spondylolesthesis are often described together.
Physical therapists provide education, pain reduction, activity modification, and cross-training to aid healing for patients with these conditions. A physical therapist can help you increase your spine and leg flexibility, strengthen your core muscles, and return to your sport, work, and recreational activities without a recurrence of symptoms.
What are Stress Fractures of the Lumbar Spine?
Spondylolysis is a stress fracture of the pars interarticularis, part of the bony ring that connects the front part of the spinal column to its back portion. Specifically, the fracture occurs between the spinous process (bony protrusion that sticks out the back of the spine) and the transverse process (bony protrusion that sticks out of the side of the spine). Excessive strain on the lumbar vertebrae due to repetitive activities in a growing child can cause injury to the vertebrae, resulting in low back pain.
Spondylolisthesis is the forward slip of a defective, unstable vertebrae. There are five grades of slips, with grade I being the smallest amount of slip and grade V being a slip of 100%. Nonsurgical management is most successful with patients who have a defect on only 1 side of the vertebrae and those patients with a grade II or less slip. Young athletes whose adolescent growth spurt has not yet occurred are at greater risk for continued slippage and are monitored until they stop growing.
Key points to understand about spondylolysis and spondylolisthesis:
- Early detection and proper diagnosis of these conditions is important because return to sport or an active lifestyle can occur within 3 to 6 months with early diagnosis. With prolonged symptoms and a delayed diagnosis, healing may take up to a year.
- The majority of symptoms resolve with rest, with or without the use of a back brace or activity modifications.
- Surgery may be indicated when conservative treatment of greater than 6 months fails and debilitating symptoms persist.
- Spondylolysis and spondylolisthesis need to be ruled out in a young athlete who is experiencing low back pain for more than a few weeks. Active young athletes who participate in sports, such as football, hockey, gymnastics, and dance are at the greatest risk of developing the conditions, especially while growing.
- A negative x-ray reading requires additional imaging to rule out early injury to the vertebrae if clinical exam findings suggest a high probability of spondylolysis.
- Spondylolysis and spondylolisthesis are not a major cause of low back pain in adults, except in high-level athletes engaging in high-risk sports.
Signs and Symptoms
Spondylolysis may be present if you are experiencing:
- Low back pain with or without buttock or leg pain (If leg pain is present, it radiates into the thigh, but generally not below the knee.)
- Muscle spasms in your low back, buttocks, and thighs
- Difficulty or pain with walking or prolonged standing
- Symptoms that are relieved by sitting, slouching, or bending forward
- Pain with sports or manual labor
- Pain with bending backwards, twisting the spine, or with throwing
- Decreased flexibility of the leg muscles
How Is It Diagnosed?
Your physical therapist will conduct a thorough evaluation that includes taking your health history. Your therapist may ask:
- How long you have had the pain, and whether it came on suddenly or gradually
- If the pain occurs with activity or at rest, or during the day or night
- What activities or positions make the pain better or worse
- If you engage in high-risk activities that may cause injury to your vertebrae
- If you can point with 1 finger to the area on your back that is painful
- If you are having any other symptoms, such as fever, chills, or night sweats
- If you have difficulty maintaining control over your bowel and bladder
Additionally, your physical therapist will perform objective tests and measures to identify movement, flexibility, or strength factors that may be contributing to your pain. Specifically, the therapist may watch you walk, have you bend forward to touch your toes, bend back as far as you can, stand on 1 leg and bend back, and turn your trunk from side to side. Your physical therapist will assess your leg and spine flexibility as well as your core strength, and ask you if the testing changes your symptoms. Your therapist may gently press areas of your back to see if they are painful. All the information gathered helps determine the cause of your pain and the best treatment to resolve your symptoms.
Diagnosing spondylolysis and spondylolisthesis can be challenging. If stress fracture is suspected, your therapist will refer you to an orthopedist or sports medicine physician familiar with back injuries. The physician may order further imaging tests to confirm the diagnosis and rule out other spine conditions.
How Can a Physical Therapist Help?
In the beginning, when you are in pain and having difficulty performing your normal daily routine, your physical therapist can:
- Show you how to rest the injured vertebrae, use lumbar bracing, modify your activities, and avoid painful movements
- Help you reduce and manage your pain symptoms
- Help you maintain fitness while healing, through pain-free cross-training, such as aquatic therapy
- Initiate symptom-free hamstring stretching and activation of your core muscles, either in or out of a back brace
When you are pain free, and the healing of your injured structures has begun, your physical therapist can help you:
- Improve the flexibility of your hip and leg muscles
- Improve your core and leg strength
- Improve your spine flexibility
- Prepare for a return to sport or work activities by improving your overall fitness levels
- Begin a gradual progression of higher-risk movements, such as back extension and trunk rotation to reduce the chance of reinjury
Can this Injury or Condition be Prevented?
Spondylolysis and some types of spondylolisthesis may be preventable by educating individuals who are at higher risk of acquiring an injury on how it can be prevented.
For the growing young athlete, monitoring exercise volume, intensity, and frequency is necessary. Coaches or parents should:
- Limit participation to 1 high-risk sport at a time during a season
- Limit participation to 1 team at a time during a season
- Enforce 1 to 2 days of rest from training per week
- Gradually increase training volume, intensity, and frequency when starting out
Additionally, bone health and overall well-being are improved by ensuring proper rest, nutrition, and hydration while participating in high levels of activity.
