-
 Injury keeping you out of the game?Our experts will get to the core of your fitness needs.OUR SERVICES
Injury keeping you out of the game?Our experts will get to the core of your fitness needs.OUR SERVICES -
 GET BACK TO THE ACTIVITIES YOU LOVEOUR SERVICES
GET BACK TO THE ACTIVITIES YOU LOVEOUR SERVICES -
 RESTORING YOUR PHYSICAL ABILITYOUR SERVICES
RESTORING YOUR PHYSICAL ABILITYOUR SERVICES -
 RESTORING YOUR QUALITY OF LIFEOUR SERVICES
RESTORING YOUR QUALITY OF LIFEOUR SERVICES -
 EVIDENCE BASED PRACTICEOUR SERVICES
EVIDENCE BASED PRACTICEOUR SERVICES -
 APPROPRIATE PROGRAM FOR A SUCCESSFUL RECOVERYOUR SERVICES
APPROPRIATE PROGRAM FOR A SUCCESSFUL RECOVERYOUR SERVICES -
 HELPING YOU ACHIEVE YOUR GOALSOUR SERVICES
HELPING YOU ACHIEVE YOUR GOALSOUR SERVICES
Cervical
Cervical radiculopathy is often referred to as a pinched nerve in the neck. It is characterized by radiating pain from the neck to the shoulder, shoulder blade, arm, or hand. Weakness and lack of coordination in the arm and hand can also occur. The condition affects an average of 85 out of 100,000 people—most often individuals in their 50s. Athletes, heavy laborers, and workers who use vibrating machinery are commonly affected. People who sit for long periods of time, or individuals with arthritis in the cervical (neck) region can also be affected. Conservative care, including physical therapy, can help reduce symptoms. A physical therapist can help alleviate the acute neck and arm symptoms that result from the condition, as well as improve general strength and function. Most cases of cervical radiculopathy are resolved with physical therapy and do not require surgery.
What is Cervical Radiculopathy?
The cervical spine consists of 7 cervical vertebrae (the bones that form the neck region). Each vertebra is separated by a gel-like disc. The discs provide shock absorption for the spine. The spinal cord travels through a canal in the cervical vertebrae. Spinal nerve roots extend from the spinal cord and branch off going to specific locations in the arm. The spinal nerves send signals to our muscles for movement as well as sensations that we feel in the entire arm. The spinal cord is like a tree trunk, and the spinal nerves are like the tree branches. If an impingement or abnormal pressure is placed on a branch near the trunk, everything along that branch will be affected.
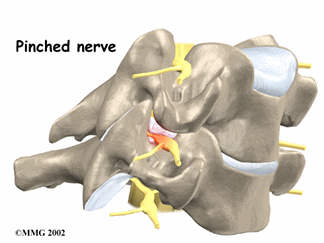
Cervical radiculopathy occurs when a nerve root coming off the spinal cord becomes compressed. The compression can occur for various reasons. In younger people, it may occur when a cervical disc herniates due to trauma. In older individuals, it commonly occurs spontaneously as a result of arthritis or decreased disc height in the neck region.
Spinal nerves can be impinged by:
- Arthritis or disc wear-and-tear with age
- Herniated or bulging discs from trauma or degeneration
- Spinal stenosis, which is a narrowing of the spaces in which the nerves travel
- Tumor, which can be benign or malignant, impinging the nerve root
When the spinal nerves are impinged, they cannot properly send messages to the muscles from the brain, nor receive proper sensation from the specific arm location the nerve travels. Everywhere the spinal nerve travels will be affected. That is why a pinched nerve in the neck can cause pain, weakness, and loss of sensation in the arm, even though the pinch is in the cervical region.
How Does it Feel?
Symptoms of cervical radiculopathy vary depending on the nerve root involved, and commonly occur on the same side of the body as the affected nerve. The symptoms may include:
- Pain in the neck, shoulder blade, shoulder, upper chest, or arm, with pain possibly radiating into the fingers following the path of the involved nerve root.
- Pain described as "sharp" or "pins-and-needles" or “popping sensation” in cervical region.
- General dull ache or numbness anywhere along the pathway of the nerve.
- Weakness in the shoulder, arm, or hand.
- Pain that worsens with certain neck movements.
- Pain that improves when the arm is lifted over and behind the head (relieving tension on the spinal nerve).
These symptoms may also be specific to the nerve root involved:
- C5 nerve root (between cervical vertebrae C4-C5): weakness in the deltoid muscle (front and side of the shoulder) and upper arm; shoulder pain and numbness
- C6 nerve root (between cervical vertebrae C5-C6): weakness in the bicep muscle (front of the upper arm) and wrist muscles; numbness on the thumb side of the hand
- C7 nerve root (between cervical vertebrae C6-C7): weakness in the triceps muscle (the back of the upper arm and wrist); numbness and tingling in the back of the arm and the middle finger of the affected hand
- C8 nerve root (between vertebrae C7-T1): weakness with hand grip; numbness in the little finger
The most common nerve root levels for this condition are C6 and C7.
How Is It Diagnosed?
When you seek the help of a physical therapist, the physical therapist performs a comprehensive evaluation and asks questions about your pain and your daily activities. These may include:
- How and when the pain started: Did the pain begin spontaneously or was there any trauma or popping experienced in the cervical region?
- Where are the symptoms located, and have they changed location or intensity since the onset?
- What makes the symptoms better or worse?
- What type of work do you perform?
- What hobbies or household activities do you regularly perform?
Your physical therapist will gently test the movement of your neck and arms. The therapist will check your tendon reflexes and strength, and conduct special tests on your neck and upper extremity to determine which spinal nerve root(s) may be involved, and to rule out other conditions. To provide a definitive diagnosis, your therapist may collaborate with an orthopedist or other health care provider. The orthopedist may order further tests, such as magnetic resonance imaging (MRI) or electromyography (EMG). An MRI can show soft tissues, including the spinal cord and nerve roots. This test can determine what is causing the compression on the nerves, including disc bulges or disc herniation. An EMG measures the nerve and muscle function. This test can tell how well your spinal nerves are communicating to your muscles.
How Can a Physical Therapist Help?
Physical therapy is an effective treatment for cervical radiculopathy, and in many cases, it completely resolves symptoms. Your physical therapist will develop an individual treatment plan based on the findings of your initial evaluation. The treatment plan may include:
Pain Management. The first goal is to reduce the pain and inflammation in the area. Ice packs applied to the neck and scapular (shoulder blade) region during the first 24 to 48 hours following the onset of pain, help reduce inflammation. Moist heat can be used after this time period to help the surrounding muscles relax. Your physical therapist may advise you to wear a soft cervical collar at times throughout the day, to allow the neck to relax. A cervical contoured pillow may be recommended to properly support the neck, and allow you to sleep more comfortably.
Manual Therapy. Your physical therapist may use manual therapy techniques, such as manual cervical traction, to relieve pressure in the cervical (neck) region. This procedure can provide immediate relief of pain and numbness radiating into the arm. Gentle massage may also be performed on the muscles of the cervical spine and scapular (shoulder blade) region. This technique helps the muscles relax and improves circulation to the area, promoting healing and pain relief.
Posture Education. Posture education is an important part of rehabilitation. Your physical therapist may suggest adjustments to your workstation and work habits, to promote good posture to protect your neck. In the early stages of recovery this may mean sitting only 15 to 20 minutes at a time. You will also receive instructions on how to bend, reach, and lift throughout the day in safe positions that place minimal pressure on your spinal discs.
Range-of-Motion Exercises. Your physical therapist will teach you gentle cervical mobility exercises to relieve your symptoms, and allow you to return to normal movement. In the beginning stages of recovery, it is important that none of these exercises increase the pain radiating down into your arm. It is important to communicate your symptoms accurately to your physical therapist. If you spend many hours sitting at a desk during your workday, your neck may become stiff. Your therapist will teach you neck stretches to take pressure off of your neck from extended periods of sitting, to help improve your mobility.
Strengthening Exercises. Your physical therapist will help you determine which muscle groups need to be strengthened based on which spinal nerves are involved in your particular case. When pain no longer radiates down your arm, you may begin more aggressive strengthening exercises. Neck stability (strengthening) exercises will also be performed. You will receive a home-exercise program to continue strengthening your neck, shoulder, arm, and upper back long after your formal physical therapy has ended.
Functional Training. As your symptoms improve, your physical therapist will work on functional exercises to help you return to your job, sport, or other daily activities. For example, if your job duties require overhead reaching, pushing, pulling, and long periods of sitting, you will be taught ways to perform these tasks to reduce undue stress to the neck.
Can this Injury or Condition be Prevented?
Your physical therapist will educate you on the best ways to prevent cervical radiculopathy from recurring, including:
- Maintaining proper posture. Use a supportive pillow and proper posture when sitting at a desk or in the car.
- Setting up your workstation to minimize undue forces on the spine. You may be advised to use a hands-free phone, or adjust your computer monitor to avoid excessive twisting or extending of your neck in repetitive directions during the workday.
- Continuing with regular exercise to maintain spinal muscles flexibility and strength, including the upper body, middle back, and core muscles.
- Keeping a healthy weight to minimize unnecessary forces on the spine.
What is a Herniated Disk?
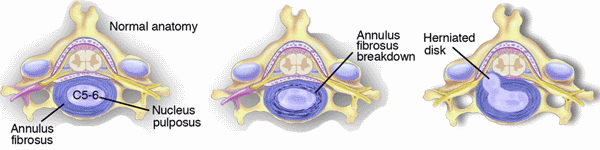
Your spine is made up of 33 vertebrae (bones) that are stacked on top of one another. Between each vertebra is a cushion-like piece of cartilage called an "intervertebral disk." Imagine the disk as a tire, with gelatin filling the hole in the tire. The rubbery outer part is called the "annulus,” and the gelatin is called the "nucleus." When we're young—under 30 years of age—the disk is made mostly of gelatin. As we age, we start to lose some of that gelatin. The disk becomes flatter and less flexible, making it easier to injure. In some cases, the gelatin can push out through a crack in the rubbery exterior and lead to a herniation (bulge) or rupture (tear).
Herniated disks are most common in the neck (cervical spine) and low back (lumbar spine). In the low back, disks may become damaged by excessive wear and tear or an injury.
Your risk for developing a herniated disk increases due to:
- Age – most herniated disks occur in people who are 30 to 50 years of age as a result of age-related disk degeneration. Herniated disks are less common after the age of 50, however, because with aging there is less fluid to push out of the disk
- Obesity – increased weight results in increased pressure on the disks
- Occupation – jobs that are physically demanding and involve repetitive tasks such as lifting, pushing, pulling, and twisting place additional stress on the disks
- Low levels of physical activity – people who are not physically active are less able to handle physical demands
Signs and Symptoms
You might have mild to intense neck or back pain—or no pain at all. Herniated disks sometimes show up on the diagnostic images of people who have no symptoms.
When the disk ruptures ("herniates") and a portion of the disk pushes outside its normal boundaries, it can "pinch" or press on spinal nerves or the spinal cord. This condition is called "radiculopathy." The pressure can lead to back pain or to pain, numbness, or weakness in the legs.
The type and location of your symptoms depends on the location and the amount of pressure on the nerves:
- If you have a herniated disk in the cervical spine, you may have pain, tingling, numbness, weakness, or any combination of these symptoms in the arm, shoulder, or neck
- If you have a herniated disk in the lumbar spine, you may have pain, tingling, numbness, weakness, or any combination of these symptoms in the back, buttocks, or legs; most likely, your symptoms will be on only one side of your body
Often, symptoms from herniated disks are made worse by certain activities or positions. If you have a herniated disk in the lumbar spine:
- Pain may get worse with sitting, bending, and reaching
- Pain may be worst first thing in the morning and after staying in one position for a long time
- You may need to switch positions frequently
- You may prefer to stand rather than sit
If you have a herniated disk in the neck, symptoms are often worse with prolonged sitting and when lying down.
How Is It Diagnosed?
Your physical therapist will conduct a thorough evaluation that includes a review of your medical history and will use screening tools to determine the likelihood of a herniated disk. For example, the therapist will:
- Ask you very specific questions about the location and behavior of your pain, weakness, and other symptoms
- Ask you to fill out a body diagram to indicate specific areas of pain, numbness, and tingling
- Perform tests of muscle strength and sensation to determine the severity of the pressure on your nerves
- Examine your posture and observe how you walk and perform other activities
- Measure the range of motion of your spine and your arms and legs
- Perform special tests, such as the straight leg raise test or the crossover straight leg raise test, that help diagnose a herniated disk
- Use manual therapy to evaluate the mobility of the joints and muscles in your spine
- Test the strength of important muscle groups
If you have muscle weakness and loss of sensation or very severe pain, special diagnostic tests, such as magnetic resonance imaging (MRI), electromyography, or nerve conduction studies may be needed. Physical therapists work closely with physicians and other health care providers to make certain that you receive an accurate diagnosis and appropriate treatment.
Research shows that in all but the most extreme cases (usually involving muscle weakness or high levels of pain), conservative care, such as physical therapy, has better results than surgery.
If your physical therapist’s evaluation indicates that there are no signs of nerve compression and you don't have any signs of muscle weakness or numbness, treatment can begin right away. If the evaluation indicates that the herniated disk might be compressing the nerves, your therapist will consult with a physician specialist.
How Can a Physical Therapist Help?
Your physical therapist's overall purpose is to help you continue to participate in your daily activities and life roles. The therapist will design a treatment program based on both the findings of the evaluation and your personal goals. Your treatment program most likely will include a combination of exercises.
Your therapist will design:
- Exercises that involve specific movements to relieve nerve pressure and decrease pain and other symptoms, especially during the early stages of treatment
- Stretching and flexibility exercises to improve mobility in the joints and the muscles of your spine, arms, and legs—improving motion in a joint can be key to pain relief
- Strengthening exercises—strong trunk muscles provide support for your spinal joints, and strong arm and leg muscles help take some of the workload off those joints
- Aerobic exercise, which has been proven to be helpful in relieving pain, promoting a healthy body weight, and improving overall strength and mobility—all important factors in managing a herniated disk
This might sound like a lot of exercise, but don't worry: research shows that the more exercise you can handle, the quicker you'll get rid of your pain and other symptoms.
Your physical therapist also might decide to use a combination of other treatments:
- Manual therapy to improve the mobility of stiff joints and tight muscles that may be contributing to your symptoms
- Posture and movement education to show you how to make small changes in how you sit, stand, bend, and lift—even in how you sleep—to help relieve your pain and help you manage your condition on your own
- Special pain treatments—such as ice, traction, and electrical stimulation—to reduce pain that is severe and not relieved by exercise or manual therapy
Once your pain is gone, it will be important for you to continue your new posture and movement habits to keep your back healthy.
Can this Injury or Condition be Prevented?
Herniated disks can occur as a result of aging, but there are lifestyle changes you can make to reduce your overall risk:
- Maintain a healthy weight may reduce the overall stress on your spine
- Use proper posture—improving your alignment may contribute to the health of your spine
- Use proper body mechanics—changing how you perform activities, especially those that you do frequently, may help reduce your risk of a herniated disk. Not sure what changes to make? Discuss your occupation with your therapist, who will provide an analysis of your job tasks and make suggestions on how you can reduce your risk of injury.
Many physical therapy clinics conduct regular educational seminars to help people in the community learn to take care of their backs and necks. These seminars often are free and provide demonstrations along with written information about exercises for the back and neck, instruction on proper lifting and sitting postures, and other tips to keep your back healthy.
If you already have a herniated disk, your physical therapist can help you develop a fitness program that takes into account your herniated disk. There are some exercises that are better than others for people with a herniated disk, and your therapist will educate you about them. For instance:
- Exercising in water can be a great way to stay physically active when other forms of exercise are painful
- Exercises involving lots of twisting and bending are not good for everyone
- Weight-training exercises, though very important, need to be done with proper form to avoid stress to the back and neck
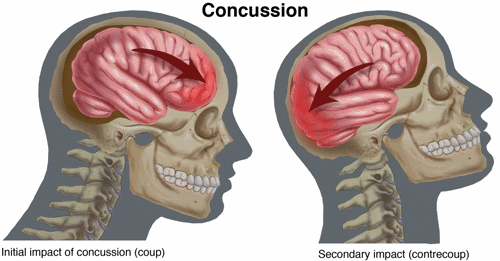
Concussion is a traumatic brain injury that can damage brain tissue and change the chemical balance of the brain. Concussion may cause physical, mental, and emotional symptoms and problems, both short-term and long-term. Every concussion is considered a serious injury by health care providers.
The Centers for Disease Control (CDC) estimates that 2.5 million concussions occurred in the United States in 2010, the most recent year for which the CDC has statistics. A physical therapist can assess symptoms to determine if a concussion is present, and treat the injury by guiding the patient through a safe and individualized recovery program.
What Is Concussion?
Concussion is a brain injury that occurs when the brain is violently shaken. This can happen during rapid movement changes (such as whiplash) or when the head is hit. This shaking or hitting of the head causes unpredictable injury to any area of the brain, resulting in immediate or delayed changes in the brain's chemistry and function. Depending on which area of the brain suffers injury, many different temporary or permanent problems with brain function can occur..
Concussions can occur at any age, from a variety of causes, including:
- Car accidents (ie, a head impact, or whiplash)
- Work accidents (ie, falls, head trauma)
- Playground accidents (ie, falling from a slide or swing)
- Sports injury to the head or neck
- Any type of fall or direct blow to the head, face, or neck
- Violent events
- physical abuse during which the head is shaken
- being too close to a blast or explosion
Recovery from a concussion can take several weeks to several months, depending on many factors, including severity and age.
Concussion may occur along with other brain injuries such as bruising, bleeding, or tearing of the brain tissue. These injuries are very severe and require the immediate care of a medical doctor, such as a neurosurgeon.
CAUTION: Concussions can be fatal or can result in permanent brain damage.
Seek medical help immediately following any head injury.
How Does it Feel?
A concussion can cause a variety of symptoms and problems in many different body functions, such as:
- The senses (eg, vision, hearing, or sense of smell problems)
- Body movements (eg, weakness or loss of balance and coordination)
- Personality and mood (eg, newly-developed irritability, depression, or trouble concentrating)
- Pain (eg, headaches or migraines)
Concussion sometimes causes loss of consciousness (“blacking out”), but not always.
Signs and Symptoms
There are many symptoms related to concussion, and they can affect your physical, emotional, and mental well-being. Some symptoms occur immediately, some a few hours after the injury, and some show up months or years after a concussion.
It is important to seek medical treatment immediately following any head injury. The risk of death or permanent brain damage from a concussion can be minimized by immediate and appropriate treatment from health care providers, like a physical therapist. Only health care providers have the knowledge and training to identify concussion in the maze of symptoms that can occur following a head injury.
Immediate and short-term symptoms
Physical symptoms:
- Headache
- Dizziness
- Difficulty with balance and coordination
- Nausea/vomiting
- Fatigue
- Difficulty sleeping
- Increased sleepiness
- Double or blurred vision
- Sensitivity to light and sound
- Slurred speech
- Glassy-eyed stare
- Seizures
Cognitive (thinking) symptoms:
- Difficulty with short-term or long-term memory
- Confusion
- Slowed "processing" (for instance, a decreased ability to think through problems)
- "Fogginess"
- Difficulty concentrating
- Worsening grades in school
Emotional symptoms:
- Irritability
- Restlessness
- Anxiety
- Depression
- Mood swings
- Aggression
- Decreased tolerance of stress
- Change in personality or behavior
Longer-term symptoms
- Loss of libido
- Loss of menses/menstruation
- Growth problems (children)
- Fatigue
- Weight gain
- Low blood pressure
- Muscle weakness
- Chronic headaches or dizziness
- Muscle spasticity
- Early dementia/chronic traumatic encephalopathy
Some concussion symptoms do not go away in the expected time frame. These symptoms may need further testing and treatment by a team of health care providers, including a physical therapist.
Postconcussion syndrome is the term applied to symptoms, such as headaches or dizziness that persist for weeks or months after the initial injury.
Second-impact syndrome is a serious, although preventable, complication that can occur after a concussion. If a person who has suffered a recent concussion experiences another concussion, permanent brain damage or death can occur. Permanent brain damage can include learning disabilities, personality changes, walking disability, or other brain or nerve disabilities. Research suggests that a person who suffers a second concussion before the initial concussion has healed, has a 100% chance of permanent brain damage, and a 50% chance of dying.
An example of second-impact syndrome would be a football player who suffers a concussion in a game, keeps playing, and is hit again; or a person who suffers a concussion from whiplash in a car accident, and then falls at home and endures another concussion very soon after the initial injury.
Extreme care should be taken after a concussion to prevent a second injury.
Athletes who suffer a concussion during practice or competition must be removed immediately from play, in order to prevent further brain damage and second-impact syndrome.
How Is It Diagnosed?
Concussion is most often diagnosed through careful testing by your health care provider, like a physical therapist. The diagnosis of concussion usually does not rely on hi-tech testing, such as an MRI or CT scan, because brain scans often do not show any brain abnormality, even when the person has symptoms of a concussion.
Your physical therapist will ask you many questions to understand all of the symptoms that you are experiencing. Your physical therapist also will perform numerous tests to identify problems caused by a concussion, including strength, coordination, balance, sight, smell, hearing, and memory tests.
During treatment, your physical therapist will repeat the same questions and tests frequently to gauge your progress and help judge when you can return to work, school, sport, or recreational activities.
If you are an athlete who underwent preseason memory (neuropsychological) testing, your physical therapist may collaborate with the health care provider who performed that testing to help determine if you have a concussion.
Your physical therapist may also examine your neck for problems following a concussion. Neck injuries can occur at the same time as concussions, and they can cause or increase headaches and dizziness.
How Can a Physical Therapist Help?
Physical therapists can evaluate and treat many problems related to concussion. Because no 2 concussions are the same, your physical therapist's examination will assess your individual symptoms and problems, so that the physical therapist can design a safe and individualized treatment program just for you. Treatment may include:
Rest and Recovery. Your physical therapist will help you and your family understand why you should limit any kind of activity (physical, sport, recreational, electronic, school) after a concussion, until it is safe to return to these activities. A period of rest helps the brain heal and helps symptoms clear up, as quickly as possible. Your physical therapist will prescribe the rest and recovery program most appropriate for your condition.
Restoring Strength and Endurance. The physical and mental rest required after a concussion can result in muscle weakness, and a decrease in physical endurance. Your physical therapist can help you regain your strength and endurance, when the right time comes, without making your concussion symptoms worse. Your physical therapist will design a therapeutic exercise program just for you, and closely monitor your symptoms as you participate in the program.
Stopping Dizziness and Improving Balance. If you have dizziness or difficulty with your balance following a concussion, a type of physical therapy called vestibular physical therapy may help. The vestibular system, which includes the inner ear and its connections with the brain, helps you keep your balance and prevent dizziness. A qualified vestibular physical therapist may be able to help reduce or stop your dizziness or balance problems after a concussion by applying special treatments or teaching you specific exercises. There even may be some simple exercises that your physical therapist can teach you to do at home.
Reducing Headaches. Your physical therapist will assess the different possible causes of your headaches, and use specific treatments and exercises to reduce and eliminate them. Treatment may include stretches, strength and motion exercises, eye exercises, hands-on techniques, like specialized massage, and the use of technologies such as electrical stimulation.
Returning to Normal Activity or Sport. As symptoms ease and you are able to regain your normal strength and endurance without symptoms returning, your physical therapist will help you gradually add normal activities back into your daily routine. Your physical therapist will help you avoid overloading the brain and nervous system, as you increase your activity level. Overloading the brain during activity after a concussion interferes with the healing of the brain tissue, and can make your symptoms return. Your physical therapist will help return you to your normal life and sport activities in the quickest and safest way possible, while allowing your brain to properly heal.
Can this Injury or Condition be Prevented?
The risk of concussion can be greatly reduced by taking the following precautions:
- Avoid motor-vehicle accidents:
- Drive defensively, not aggressively.
- Eliminate distractions while driving, such as eating, talking on a cell phone, or texting.
- Choose cars with airbags.
- Make sure the airbags in your car are in good working order.
- Avoid risky behavior in sports:
- Absolutely avoid football techniques that increase the risk of concussion, such as "spearing" and headbutting.
- Avoid or limit "heading" the ball in soccer.
- Don’t ignore or hide signs of concussion, even in an important game or competition. Report them immediately to your coach.
- Remember that neither helmets nor mouth guards prevent concussions.
- Clear your walking areas at home of any objects that might increase the risk of falling, such as loose throw rugs, dropped objects, loose flooring, torn or rumpled carpets, pet toys, or dishes.
- Make sure that all traffic areas in your home are well-lit.
- Avoid exposure to blast explosions and violent events.
- Do not shake babies, or anyone of any age!
It is imperative to prevent second-impact syndrome after an initial concussion. The injured person should be closely protected until all symptoms have cleared, and normal activity can resume.
Pain of any type that occurs in any part of the head is called a headache. There are many different types of headaches, with just as many causes. The International Headache Society describes several different categories of headache:
- Tension-type
- Migraine and cluster
- Secondary headaches from an underlying condition, such as fever, infectious disease, sinus disorder, or in rare cases, a tumor or more serious illness
- Cranial neuralgias, facial pain, and other headaches
Most headaches are harmless and resolve on their own, although severe headaches that recur frequently can affect your ability to do your daily activities and can reduce your quality of life.
There is effective treatment for almost every type of headache. The challenge lies in determining the type of headache, its cause, and in developing an appropriate treatment plan that will reduce both its frequency and intensity. Physical therapists can help determine the type of headache you have and are experts in managing pain from tension-type headaches.
What are Headaches?
Headaches, like back pain, are one of the most common of all physical complaints and can be one of the most frustrating to manage. Pain of any type that occurs in any part of the head is called a headache.
Tension-type headaches (also called muscle-spasm headaches) are the most common types of headaches in adults. They may be the result of a neck or jaw problem, poor posture, fatigue, or stress.
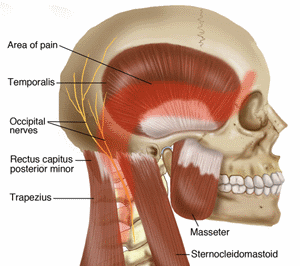
A problem in the neck, head, or jaw--such as an injury or arthritis--can lead to tension in the muscles at the back of the head and to increased pressure on the nerves to the face and head. Poor posture can cause these muscles to become overworked, which can trigger a headache.
How Does it Feel?
A tension-type headache typically begins at the back of the head and spreads to the top of the head and the eyes. You might feel an increase in facial pain along the cheeks near the jaw bone (temporomandibular joint dysfunction). People often describe tightness, a sensation of someone tugging on their hair, or a feeling of wearing a tight cap. These headaches can worsen with specific positions--such as sitting at a desk--and may ease with rest.
How Can a Physical Therapist Help?
Your physical therapist will conduct a thorough examination that includes a review of your health history. Your therapist will ask you questions and will perform tests to determine the most likely cause of your headaches. For example, your therapist might:
- Ask you:
- to recall any previous injuries to your neck, head, or jaw
- the location, nature, and behavior of your pain and other symptoms
- to draw your areas of pain on a body diagram
- Perform tests of muscle strength and sensation
- Examine your posture when sitting, standing, and performing various activities
- Measure the range of motion of your neck, shoulders, and other relevant parts of your body
- Use manual therapy to evaluate the mobility of the joints and muscles in your neck
If it appears that you do have tension-type headaches, your physical therapist will work with you to design a plan of care to meet your goals. If the evaluation indicates that you may have a different type of headache--such as sinus, migraine, or cluster headache--your physical therapist likely will refer you to another health care professional for additional diagnostic tests and treatment.
Your physical therapist will work with you to correct the problems that are causing your pain and will help you learn to prevent headaches through simple changes in your posture and lifestyle:
Improve neck mobility. Physical therapists use a specialized technique called manual therapy to increase movement and relieve pain and to stretch the muscles of the back of the neck.
Improve your strength. Your physical therapist will teach you exercises to increase the strength of the muscles that help stabilize your upper back and neck to improve your posture and endurance and make it easier for you to sit or stand for longer periods of time without discomfort.
Improve your posture. Physical therapists will teach you to ways to improve your posture. Whether it is simply pushing your chest out or pulling your shoulder blades backward and together, slight modifications to everyday living can make a vast improvement in posture.
Modify your workstation or home office. Tips may include:
- using a headset instead of a regular phone
- adjusting your computer screen so that it is no lower than the level of your eyes
- finding an appropriate desk chair
- adjusting the position of your computer mouse
Torticollis is a condition that occurs when the muscle that runs up and toward the back of the neck becomes tight, weakened, or thickened, causing the head to tilt; the chin points toward one shoulder while the head tilts toward the opposite shoulder. The most common form of this condition is congenital muscular torticollis (CMT), which affects infants and is generally diagnosed within the first 2 months of life; however, torticollis also can occur in adults.
In 1992, the American Academy of Pediatrics began their "Back to Sleep" campaign to reduce Sudden Infant Death Syndrome (SIDS). The campaign successfully decreased SIDS by 40% in the United States, but it had an unintended result of contributing to the development of CMT in about 1 in every 250 infants. (Talk to your family physician and/or pediatrician if you have any questions about the "Back to Sleep" campaign.
If symptoms such as trouble breathing or swallowing, weakness in the arms or legs, impaired speech, difficulty walking, a pins-and-needles feeling or numbness in the arms or legs, or urinary or fecal incontinence accompany the head tilt—seek immediate medical attention.
What is Torticollis?
Torticollis is the tilt and/or rotation of the head because of tight and weak neck muscles. It occurs when the muscle that runs up and toward the back of the neck (the sternocleidomastoid muscle) becomes tight, weakened, or thickened. There are 5 forms of the condition:
- Congenital muscular torticollis (CMT) is the most common form of the condition. It affects infants and is generally diagnosed within the first 2 months of life. CMT is often caused by birth trauma, or by sleeping or remaining in 1 position for a prolonged period of time.
- Postural torticollis is diagnosed when the infant’s head tilt comes and goes. It is diagnosed within the first 5 months of life and often is the result of a lack of a variety of positions.
- Ocular torticollis is caused by a vision problem in 1 eye, causing the individual to tilt his or her head to see better.
- Spasmodic torticollis (wryneck) occurs in older children and adults. It can be caused by infection, inflammation, trauma, or the side effects of certain medications and/or drugs such as Ketamine, Cocaine, Prochlorperazine, Haloperidol, Chlorpromazine, and amphetamines.
- Acute torticollis occurs when a child or adult bends or twists the neck too far, or experiences some type of trauma. There may be pain when the head is moved from side to side or up and down; the neck muscle may be tender to touch.
- Osseous abnormalities are caused by improper alignment of the cervical spine (at the spinal points C1-C2) when ligaments are damaged due to an infection. The types of infection that can cause this condition include: severe upper respiratory, ear, or sinus infections; or cervical adenitis and cervical abscess. Any inflammatory process that irritates the muscles, nerves, or vertebrae—including surgery or trauma—can produce a reflex spasm resulting in this form of torticollis.
- Neurogenic abnormalities cause an acute episode of a condition that usually occurs in older children, such as a spinal cord tumor or progressive spinal cord diseases. Children will experience headaches, vomiting, and positive neurological signs. Seek immediate medical attention if any of these symptoms occur.
Torticollis may lead to additional problems, such as:
- Flattening of the skull (phylagocephaly) in infants
- Movement that favors 1 side of the body, affecting the arms, trunk, and hips. This can lead to strength imbalances, such as an elevated shoulder and side-bending of the trunk.
- Developmental hip dysplasia
- Scoliosis
- Limited ability to turn the head to see, hear, and interact with surroundings, which can lead to delayed cognitive development
- Delayed body awareness or lack of self-awareness and interaction
- Difficulty with balance
Signs and Symptoms
An adult, child, or infant may keep the head tilted and/or rotated toward 1 side of the body as attempting to straighten the neck is difficult or painful. For example, if the muscle on the left side of the neck is shortened, weak, or in spasm—the head may tilt toward the left shoulder and rotate toward the right.
There may be tightness in the neck or a noticeable lump in the neck muscle. Pain may or may not be present, depending on the type of torticollis.
How Is It Diagnosed?
Torticollis in adults is generally diagnosed by physicians. Experienced pediatric physical therapists may diagnosis the need for treatment of congenital muscular torticollis and positional torticollis.
Once the type of torticollis is determined, your physical therapist may provide treatment. In most cases, torticollis is a muscular problem, and physical therapists are musculoskeletal experts.
How Can a Physical Therapist Help?
Regardless of the patient’s age, physical therapy is the primary treatment for all forms of torticollis. Physical therapists provide treatment to address the impairments that are caused by torticollis. Early treatment results in the best outcomes.
The physical therapist will work with a child’s caregiver or with an adult patient to develop and reach mutual goals. This may include an individualized treatment plan to:
- Strengthen neck muscles
- Correct muscle imbalance
- Gain pain-free movement (range of motion)
- Improve postural control and symmetry
- Improve the body’s alignment by easing muscle tension
These goals may be achieved through stretching, strengthening, massage, positioning, taping, and a home exercise program. If not treated, torticollis can become a permanent condition.
