-
 Injury keeping you out of the game?Our experts will get to the core of your fitness needs.OUR SERVICES
Injury keeping you out of the game?Our experts will get to the core of your fitness needs.OUR SERVICES -
 GET BACK TO THE ACTIVITIES YOU LOVEOUR SERVICES
GET BACK TO THE ACTIVITIES YOU LOVEOUR SERVICES -
 RESTORING YOUR PHYSICAL ABILITYOUR SERVICES
RESTORING YOUR PHYSICAL ABILITYOUR SERVICES -
 RESTORING YOUR QUALITY OF LIFEOUR SERVICES
RESTORING YOUR QUALITY OF LIFEOUR SERVICES -
 EVIDENCE BASED PRACTICEOUR SERVICES
EVIDENCE BASED PRACTICEOUR SERVICES -
 APPROPRIATE PROGRAM FOR A SUCCESSFUL RECOVERYOUR SERVICES
APPROPRIATE PROGRAM FOR A SUCCESSFUL RECOVERYOUR SERVICES -
 HELPING YOU ACHIEVE YOUR GOALSOUR SERVICES
HELPING YOU ACHIEVE YOUR GOALSOUR SERVICES
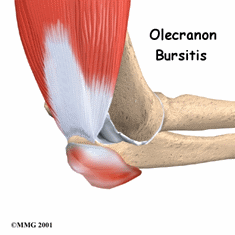
Elbow
Elbow (olecranon) bursitis, commonly known as "baker's elbow," "student's elbow," or "Popeye elbow," involves swelling at the tip of the elbow, on the back of the arm. The condition can be painless, or it can be painful at rest and when leaned on, as when writing with the arm pressing on a table. Elbow bursitis can have many causes, but the most common is trauma, whether a direct hit, or smaller bumps or pressure applied over time. Elbow bursitis is commonly seen in students or office workers who lean their elbows on hard desks or armrests for long periods of time; however, its occurrence is not related to any particular age or ethnic group. The condition can also be caused by infection or autoimmune conditions. Sometimes, however, a specific cause cannot be determined. Physical therapists treat individuals with elbow bursitis to reduce their pain, swelling, stiffness, and any associated weakness in the elbow or upper extremity.
What is Elbow Bursitis?
Elbow bursitis (also called olecranon bursitis) occurs when the bursa (a fluid-filled sac on the tip of the elbow) becomes damaged, irritated, or inflamed. Normally, the bursa acts as a cushion for the tip of the elbow (ulna) bone. Certain types of pressure, traumatic blows, or repetitive motions can cause constant friction or irritation of the bursa, leading to the development of bursitis ("itis" means "inflammation of"). When the bursa becomes injured, it can swell and become painful.
Elbow bursitis can be caused by:
- Repetitive motions (playing sports, such as tennis or golf; prolonged leaning on the elbows, as when typing on a computer keyboard)
- Direct trauma (being hit or falling on the tip of the elbow)
- Elbow surgery or replacement
- Infection
- Autoimmune conditions
How Does it Feel?
With elbow bursitis, you may experience:
- Swelling on the tip or back of the elbow
- Redness on the tip of the elbow
- Pain when you push with your fingers on the tip of the back of the elbow
- Pain when leaning on the arm, as when the arm is resting on an armrest or on the edge of a desk or table
- Stiffness in the elbow joint, and difficulty bending the elbow
How Is It Diagnosed?
If you see your physical therapist first, your physical therapist will conduct a thorough evaluation that includes taking your health history. Your physical therapist will also ask you detailed questions about your injury, such as:
- How and when did you notice the swelling and/or pain?
- Have you been performing any repetitive activity?
- Did you receive a direct hit to the elbow, fall on it, or lean on it for a long period of time?
Your physical therapist also will perform special tests to help determine the likelihood that you have elbow bursitis. Your physical therapist will gently press on the back side of the elbow to see if it is painful to the touch, and may use additional tests to determine if other parts of your elbow are injured. Your therapist also will observe how you can move your elbow and arm, and test your strength and flexibility.
Your physical therapist will test and screen for other, more serious conditions that could cause elbow pain or swelling. To provide a definitive diagnosis, your physical therapist may collaborate with an orthopedic physician or other health care provider, who may order further tests, such as an x-ray to confirm the diagnosis and to rule out other damage to the elbow, such as a fracture or infection.
How Can a Physical Therapist Help?
Your physical therapist will work with you to design a specific treatment program that will speed your recovery, including exercises and treatments that you can do at home. Physical therapy will help you return to your normal lifestyle and activities. The time it takes to heal the condition varies, but results can be achieved in 2 to 8 weeks or less, when a proper swelling management, stretching, and strengthening program is implemented.
During the first 24 to 48 hours following your diagnosis, your physical therapist may advise you to:
- Apply light compression by wrapping the elbow a specific way, using a compressive wrap.
- Rest the area by avoiding any activity that causes pressure or pain on the elbow.
- Apply ice packs to the area for 15 to 20 minutes every 2 hours.
- Consult with a physician for further services, such as medication or diagnostic tests.
Your physical therapist will work with you to:
Reduce Pain and Swelling. If repetitive activities have caused the elbow bursitis, your physical therapist will help you understand how to avoid or modify the activities, to allow healing to begin. Your physical therapist may use different types of treatments and electrothermal modalities to control and reduce your pain and swelling
Improve Motion. Your physical therapist will choose specific activities and treatments to help restore normal movement in the elbow and arm. These might begin with "passive" motions that the therapist performs for you to gently move your elbow joint, and progress to active exercises and stretches that you do yourself.
Improve Flexibility. Your physical therapist will determine if any of your arm muscles are tight, start helping you to stretch them, and teach you how to stretch them.
Improve Strength. If your physical therapist finds any weak or injured elbow muscles, your therapist will choose, and teach you, the correct exercises and equipment to steadily restore your strength and agility.
Improve Endurance. Restoring your arm's muscular endurance is important after an injury. Your physical therapist will develop a program of activities to help you regain the endurance you had before the injury, so you can return to doing the things you like to do.
Learn a Home Program. Your physical therapist will teach you strengthening and stretching exercises to perform at home. These exercises will be specific for your needs; if you do them as prescribed by your physical therapist, you can speed your recovery.
Return to Activities. Your physical therapist will discuss your activity goals with you and use them to set your work, sport, and home-life recovery goals. Your treatment program will help you reach your goals in the safest, fastest, and most effective way possible. Your physical therapist will teach you exercises, work retraining activities, and sport-specific techniques and drills to help you achieve your goals.
Speed Recovery Time. Your physical therapist is trained and experienced in choosing the best treatments and exercises to help you safely heal, return to your normal lifestyle, and reach your goals faster than you are likely to do on your own.
If Surgery Is Necessary
Surgery is not commonly required for elbow bursitis, but if surgery is needed, you will follow a recovery program over several weeks, guided by your physical therapist. Your physical therapist will help you minimize swelling and pain, regain motion and strength, and return to normal activities in the safest and speediest manner possible.
Can this Injury or Condition be Prevented?
Your physical therapist can recommend a home program to help prevent elbow bursitis. It may include strength and flexibility exercises for the arm muscles.
To help prevent a recurrence of the injury, your physical therapist may advise you to:
- Avoid leaning on your elbow as much as possible.
- Use a wrist guard/pad on your desk to cushion your elbow when you do lean on it.
- Use a proper typing arm position that does not involve leaning on the elbows.
- Avoid hard hits or prolonged pressure to the tip of the elbow.
- Use elbow pads during sports or other physically challenging activities to protect your elbow.
- Follow a consistent flexibility and strengthening exercise program, especially for the elbow muscles, to maintain good physical conditioning, even in a sport's off-season.
- Always warm up before starting a sport or heavy physical activity.
- Gradually increase any athletic activity, rather than suddenly increasing the activity amount or intensity.
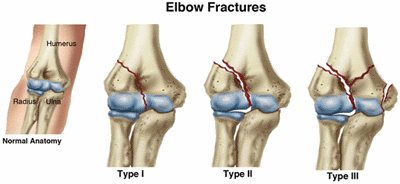
An elbow fracture is a bone break that occurs in the middle of the arm, in the area of the elbow joint. Its main cause is trauma, such as falling on the elbow, or falling on an outstretched hand. An elbow fracture can happen to anyone. Recent studies have identified a high number of fractures among children, women, and the elderly. Children have the highest rate of elbow fracture: 30 out of every 10,000 children in the United States are affected. Elbow fractures are diagnosed in 7.4 out of every 10,000 American adults, with lower-income adults also highly affected. Athletes frequently experience elbow fractures.
Physical therapists design individualized treatment programs for people with elbow fractures that help improve elbow movement and strength, ease swelling, and restore use of the arm for daily living and athletic activities. They also help prevent problems in other arm areas (hand, wrist, shoulder) that can occur when the elbow is immobilized in a cast or splint.
What is an Elbow Fracture?
Elbow fractures are bone breaks that can happen in any of the 3 bones in the area of the elbow joint (humerus, radius, or ulnar bones). Often, a person will feel or hear a snap or pop in the elbow area at the time of the injury. An elbow fracture can happen from falling on or being hit in the hand, wrist, elbow, or shoulder. The fracture can be a crack in the bone, a bone chip, or a more serious splitting of the bone.
There are 3 types of bone fractures:
- Type I. A "nondisplaced" fracture, where the bone has a break, but is still in its normal position.
- Type II. A fracture where a fragment of bone is shifted from its normal position.
- Type III. The most serious type of fracture, with multiple breaks of the bone.
Type I and II fractures usually are treated without surgery, but Type III fractures usually require surgery. Fractures can take 2 to 8 weeks or more to heal, depending on their severity and on each affected individual’s general health.
Physical therapy can help speed recovery from all types of elbow fracture, including those that require surgery.
How Does it Feel?
If you have an elbow fracture, you may experience:
- Moderate to severe pain. It’s usually too painful to move the arm.
- Tightness, stiffness, or cramping in the arm.
- Swelling, throbbing, redness, or numbness in the area.
- A grinding or catching sensation at the elbow.
- An unusual shape to the bones in the area (deformity).
- Tenderness to touch. The area also may feel hot.
- Numbness in the elbow, forearm, wrist, or hand. If you experience sudden numbness and weakness in your forearm or hand after an elbow fracture, it could indicate nerve compression. See a physician immediately!
How Is It Diagnosed?
If a physical therapist suspects that you have an elbow fracture, your therapist will refer you to a physician, who may order an x-ray. Your physical therapist can check for damage to other joints and muscles, and make sure that the nerves and blood vessels in your arm have not been affected by the broken bone.
In most cases, people with fractures visit a physician with a specialty in managing bones and joints (orthopedist). Depending on the type of fracture, the physician might prescribe a cast or a sling, or, with severe fractures, surgery.
How Can a Physical Therapist Help?
Following an elbow fracture, your physical therapist will design an individualized treatment program to help improve your elbow movement and strength, ease swelling, and restore use of your arm for daily living and athletic activities.
While Your Elbow Is in a Cast or a Sling
While your bone heals, your arm will be in a cast or a sling to keep it still and allow healing. This is also the case if you have had surgery. During the healing process, it is important to prevent as much stiffness, weakness, or swelling as possible. Depending on the amount of activity that is allowed by your physician for your type of fracture or surgery, your physical therapist will prescribe exercises to keep your shoulder, wrist, and hand moving while you are in the cast or sling.
Your physical therapist will help you stay as independent as possible by teaching you how to perform your daily activities—such as dressing, working on a computer, housekeeping, and even exercising—while wearing a cast or a sling. Under your physical therapist’s guidance, you can exercise your other arm and legs to maintain and build your fitness level during the healing process.
When the Cast or Sling Is Removed
When your cast or sling is removed, your elbow will most likely be stiff and your arm will be weak, especially if you have had surgery. Your physical therapist will help you prevent permanent loss of movement in the elbow, so don't delay your visit! Your therapist will examine your elbow and select treatments based on your particular physical problems, goals, level of physical activity, and general health.
Your physical therapist may prescribe treatments to help you:
Reduce Pain and Swelling. Your physical therapist may use different types of treatments and electrothermal modalities, such as specialized massage, electrical stimulation, and cold packs to reduce pain and swelling.
Improve Your Ability to Move. Your physical therapist will choose specific activities and treatments to help restore normal movement in the elbow and arm. These might begin with "passive" motions that your therapist performs for you to gently move your elbow joint, and progress to active exercises and stretches that you do yourself.
Increase Flexibility. Your physical therapist may gently apply hands-on treatment (manual therapy) to enable your joints and muscles to move more freely with less pain. These techniques can include stretches and therapeutic massage techniques.
Increase Strength. If your physical therapist finds any weakness in your arm or hand muscles, your therapist will choose, and teach you, the correct exercises and equipment to steadily restore your strength and agility. You might use equipment, such as therapy bands, therapy putty, and hand weights to help strengthen your arm.
Improve Endurance. Restoring your arm's muscular endurance is important after an injury. Your physical therapist will develop a program of activities to help you regain the endurance you had before the injury, so you can return to doing the things that you like to do.
Learn a Home Program. Your physical therapist will teach you strengthening and stretching exercises to perform at home. These exercises will be specific for your needs; if you do them as prescribed by your physical therapist, you can speed your recovery.
Return to Activities. Your physical therapist will discuss your activity goals with you and use them to set your work, sport, and home-life recovery goals. Your treatment program will help you reach your goals in the safest, fastest, and most effective way possible. Your physical therapist will teach you exercises, work retraining activities, and sport-specific techniques and drills to help you achieve your goals.
Speed Recovery Time. Your physical therapist is trained and experienced in choosing the best treatments and exercises to help you safely heal, return to your normal lifestyle, and reach your goals faster than you are likely to do on your own.
Can this Injury or Condition be Prevented?
Your physical therapist can recommend a few ways to prevent elbow fractures, including:
- Avoiding hard hits to the elbow, shoulder, or hand.
- Avoiding falls or other trauma to the arm. Your physical therapist is an expert at determining your risk of falling, and can teach you how to perform balance exercises to lower that risk. Your therapist also can teach you how to decrease the risk of falling in your home and community by:
- Clearing floors of loose items and throw rugs.
- Lighting dark hallways.
- Keeping pets away from your feet when walking.
- Practicing simple balance techniques.
- Avoiding walking in icy areas.
- Wearing nonslip shoes/boots during wintry weather conditions.
- Walking carefully near “wet floor” signs.
- Using protective equipment during sports, such as wrist guards or elbow pads.
- Learning safer falling positions and techniques for sports.
- Always warming up before starting a sport or heavy physical activity.
- Gradually increasing the amount or intensity of any athletic activity.
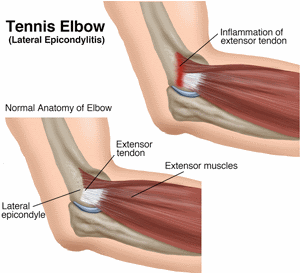
Tennis Elbow (Lateral Epicondylitis)
Most people who get tennis elbow don't play tennis! In fact, less than 5% of all cases of tennis elbow occur in people who play tennis. Tennis elbow can happen to anyone who repeatedly uses their elbow, wrist, and hand for their job, sport, or hobby.
What Is Tennis Elbow (Lateral Epicondylitis)?
Tennis elbow is a painful condition caused by overuse of the "extensor" muscles in your arm and forearm, particularly where the tendons attach to rounded projections of bone (epicondyles) on the outside or lateral aspect of the elbow. The muscles you use to grip, twist, and carry objects with your hand all attach to the "lateral epicondyle" at the elbow. That's why a movement of the wrist or hand can actually cause pain in the elbow.
Prolonged use of the wrist and hand, such as when using a computer or operating machinery —and, of course, playing tennis with an improper grip or technique—can lead to tennis elbow. It can happen to athletes, non-athletes, children, and adults. It occurs more often in men than women, and most commonly affects people between the ages of 30 and 50.
Signs and Symptoms
Symptoms of tennis elbow can occur suddenly as a result of excessive use of the wrist and hand for activities that require force, such as lifting, twisting, or pulling. Forceful activities—like pulling strongly on a lawn mower starter cord—can injure the extensor muscle fibers and lead to a sudden onset of tennis elbow.
More commonly, though, symptoms of tennis elbow develop gradually over a period of weeks or months as a result of repeated or forceful use of the wrist, hand, and elbow. If you work as a grocery store cashier, you might have symptoms of tennis elbow as a result of repetitive (and often too forceful) typing—combined with continuous lifting of grocery bags.
Your symptoms may include:
- Pain that radiates into your forearm and wrist
- Difficulty doing common tasks, such as turning a doorknob or holding a coffee cup
- Difficulty with gripping activities
- Increased pain when you use your wrist and hand for lifting objects, opening a jar, or gripping something tightly, such as a knife and fork
- Stiffness in the elbow
- Weakness in the forearm, wrist, or hand
How Is It Diagnosed?
Tennis elbow usually occurs due to repeated movements. As a result, other muscles and joints in this region of the body may be affected as well. Your physical therapist will perform a careful examination not only of your elbow but of other areas of your body that might be affected and might be contributing to your pain. Your therapist will perform special manual tests that help diagnose the problem and help detect conditions such as muscle weakness that might have led to the problem in the first place. For instance, the therapist might ask you to gently tense or stretch the sore muscles to identify the exact location of the problem. Rarely is an x-ray required to diagnose this condition.
How Can a Physical Therapist Help?
The First 24 to 48 Hours
For the first 24 to 48 hours after acute onset of your pain, treatment includes:
- Resting the arm by avoiding certain activities and modifying the way you do others
- Using 10-20 minute ice treatments
- Using elastic bandages or supports to take the pressure off of the painful muscles
Your physical therapist will decide if you should use a brace or support to protect your muscles while the area is healing. Depending on severity, your therapist may recommend that you consult with another health care provider for further testing or for consideration of additional treatment such as medication. In rare cases, treatments such as cortisone injection or surgery might be needed. Your physical therapist can help you determine whether you need a referral to another health care provider.
Your physical therapist can design a specific treatment program to speed your recovery. There will very likely be exercises and other treatments that you will be expected to do at home. Your physical therapist also might use special physical therapy treatments to help relieve pain, such as manual therapy, special exercises, and ice or heat treatments or both.
For an "acute" case of tennis elbow—one that has occurred within the past few weeks— it's important to treat as early as possible. Left untreated, tennis elbow may become chronic and last for months and sometimes even years. This is especially true if treatment is focused only on relieving pain and not on correcting the muscle weakness and bad habits that might have led to your condition in the first place.
Improve Your Ability to Move
Your physical therapist may use manual therapy to enable your joints and muscles to move more freely with less pain.
Improve Your Strength
Insufficient muscle strength can lead to tennis elbow. Sometimes the weakness is in the muscles of the wrist and forearm. In many cases, the problem stems from weakness of the supporting postural, or "core," muscles. In fact, you might find that it is necessary to improve your overall level of fitness to help manage your elbow condition. Based on the evaluation, your physical therapist can determine the type and amount of exercises that are right for you.
Physical therapists prescribe several types of exercises during recovery from tennis elbow:
- Early in the treatment, when the pain is most intense, your therapist may recommend passive exercises in which your wrist and elbow are moved without the use of your muscles.
- As your symptoms improve, you can move the wrist and elbow actively without assistance.
- As the muscles become stronger and the symptoms have lessened, you will be able to begin using weights or resistance bands to further increase your strength. The amount of weight will need to be carefully monitored to make sure you continue to progress and avoid re-injuring your muscles.
Use Your Muscles the Right Way
Your physical therapist can help you retrain your muscles so that you use them properly. For example, when you lift a heavy grocery bag, you should contract the muscles around your shoulder blade and trunk to provide support for your arm muscles. This simple movement can be easily taught to you by a physical therapist can lessen the stress to the injured muscles and help you return to your normal activities while avoiding re-injury.
Return to Your Activities
Your physical therapist will help you remain active by teaching you how to modify your daily activities to avoid pain and further injury. Sometimes it's necessary to make changes at work, on the playing field, or in the home. Your physical therapist can help you make simple modifications to your work site, your computer set-up, your kitchen devices, your sports equipment, and even your gardening tools to lessen the strain to your hand, wrist, and forearm. Your therapist will emphasize the importance of taking stretch breaks so that your muscles get frequent rest from repetitive movements and standing or sitting in the same position.
Tennis may be a contributing factor to tennis elbow for several reasons. Sometimes the problem results from over-training. In other cases, the weight of the racquet or its grip may need to be adjusted. For others, the problem may stem from improper form, poor overall fitness, or a lack of strength in the supporting or "core" muscles of the trunk and shoulder blades. A physical therapist can help analyze the source of the problem and help find a solution.
Can this Injury or Condition be Prevented?
Yes! You can help prevent tennis elbow by staying fit, using proper technique in your sport or in your job, and using equipment that is well designed and appropriate for your body type and your level of activity. Your physical therapist can show you how. If you had tennis elbow years ago, you might be at risk for re-injury if the tendons did not have time to completely heal or if your muscle strength and joint mobility were not fully restored. Returning to sports or activities before you have fully recovered might result in an elbow that has persistent pain or is easily or frequently re-injured. A physical therapist can help determine when you are ready to return to your activities and sports and can help make sure that your elbow, forearm, and wrist are strong and ready for action.
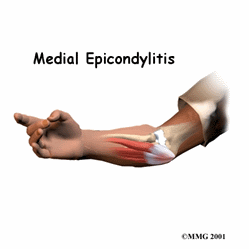
Medial Epicondylitis (Golfer's Elbow)
Medial epicondylitis (commonly called golfer's elbow or thrower's elbow) is a condition that develops when the tendons on the inside of the forearm become irritated, inflamed, and painful due to repetitive use of the hand, wrist, forearm and elbow. It is often diagnosed in people who perform repetitive motions, such as swinging a golf club or tennis racket, or activities requiring gripping, twisting, or throwing. Even using a computer or performing yard work can cause the condition. It is most common in men over the age of 35. A physical therapist can help decrease the pain caused by medial epicondylitis, and improve the affected elbow's motion, strength, and function.
What is Medial Epicondylitis (Golfer's Elbow)?
Medial epicondylitis is a condition that occurs when the tendons on the inside of the forearm become irritated, inflamed, and painful due to repetitive use of the hand, wrist, and forearm. A tendon is a soft tissue that attaches a muscle to a bone. The group of muscles affected by medial epicondylitis are those that function to flex (bend) the wrist, fingers, and thumb and pronate (rotate palm-down) the wrist and forearm. The muscle group comes together into a common sheath and attaches to the humerus bone of the upper arm. This bony prominence, called the medial epicondyle, is located along the inside of the elbow. Pain occurs on or near the medial epicondyle, at the area where the tendon connects to the bone. Repetitive forces can cause the tendon to become tender and irritated, and without treatment, can cause it to even tear away from the bone. In addition, as the muscle groups travel across both the elbow and the wrist, they function to stabilize at the elbow allowing for wrist movement. As this is a 2-joint tendon, it is more vulnerable to injury.
How Does it Feel?
Persons with medial epicondylitis may experience:
- Pain along the inside of the forearm with wrist, hand, or elbow movements.
- Pain or numbness and tingling that radiates from the inside of the elbow down into the hand and fingers, with gripping or squeezing movements.
- Tenderness to touch and swelling along the inside of the forearm.
- Weakness in the hand and forearm when attempting to grip objects.
- Elbow stiffness.
How Is It Diagnosed?
Your physical therapist will perform an evaluation and ask you questions about pain or other symptoms you are feeling. Your physical therapist may perform strength and motion tests on your wrist, forearm, and elbow; ask about your job duties and hobbies; evaluate your posture; and check for any muscle imbalances and weakness that can occur anywhere along the path from your shoulder blade to your hand. Your physical therapist will gently touch your elbow in specific areas to determine which tendon or tendons may be inflamed. Special muscle tests, such as bending the wrist or rotating the forearm with resistance, also may be performed to ensure a proper diagnosis.
How Can a Physical Therapist Help?
It is important to get proper treatment for medial epicondylitis as soon as it occurs, as tendons do not have a good blood supply. An inflamed tendon that is not treated can begin to tear, causing a more serious condition.
When a diagnosis of medial epicondylitis is made, you will work with your physical therapist to devise a treatment plan that is specific to your condition and goals. Your individual treatment program may include:
Pain Management. Your physical therapist will help you identify and avoid painful movements to allow the inflamed tendon to heal. Ice, ice massage, or moist heat may be used for pain management. Therapeutic modalities, such as iontophoresis (medication delivered through an electrically charged patch), and ultrasound may be applied. Bracing or splinting may also be prescribed. In severe cases, it may be necessary to rest the elbow and not perform work or sport activities that continue causing pain, which may slow the recovery process.
Pain Management. Your physical therapist will help you identify and avoid painful movements to allow the inflamed tendon to heal. Ice, ice massage, or moist heat may be used for pain management. Therapeutic modalities, such as iontophoresis (medication delivered through an electrically charged patch), and ultrasound may be applied. Bracing or splinting may also be prescribed. In severe cases, it may be necessary to rest the elbow and not perform work or sport activities that continue causing pain, which may slow the recovery process.
Pain Management. Your physical therapist will help you identify and avoid painful movements to allow the inflamed tendon to heal. Ice, ice massage, or moist heat may be used for pain management. Therapeutic modalities, such as iontophoresis (medication delivered through an electrically charged patch), and ultrasound may be applied. Bracing or splinting may also be prescribed. In severe cases, it may be necessary to rest the elbow and not perform work or sport activities that continue causing pain, which may slow the recovery process.
Manual Therapy. Your physical therapist may use manual techniques, such as gentle joint movements, soft-tissue massage, and elbow, forearm, and wrist stretches to help the muscles regain full movement. Your therapist may also do manual stretching and manual techniques to your shoulder and thoracic spine, as your tendons along the medial elbow can be affected by muscle imbalances all the way up the chain.
Range-of-Motion Exercises. You will learn mobility exercises and self-stretches to help your elbow and wrist maintain proper movement.
Strengthening Exercises. Your physical therapist will determine which strengthening exercises are right for you, depending on your specific condition, as your pain subsides. You may use weights, medicine balls, resistance bands, and other types of resistance training to challenge your weaker muscles. You will receive a home-exercise program to maintain your arm, forearm, elbow, and hand strength long after you have completed your formal physical therapy.
Patient Education. Education is an important part of rehabilitation. Your physical therapist may suggest adjustments to how you perform various tasks, and make suggestions to improve your form and reduce any chance of injury. Adjustments made in your golf swing, throwing techniques, or work tasks can help reduce pressure placed on the tendons in the forearm region.
Functional Training. As your symptoms improve, your physical therapist will help you return to your previous level of function. Functional training will include modifications in specific movement patterns, promoting less stress on the medial tendons. As mentioned previously in patient education, you and your physical therapist will decide what your goals are, and safely get you back to your prior performance levels as soon as possible.
Can this Injury or Condition be Prevented?
Understanding the risk of injury and being aware of your daily movements can help prevent the development of medial epicondylitis. Individuals should:
- Maintain proper form and technique when performing repetitive work tasks or sports movements, like golf swings.
- Maintain shoulder, forearm, and wrist muscle strength.
- Perform gentle forearm muscle stretches before and after performing tasks.
- Use proper posture and body mechanics when lifting heavy objects to reduce joint strain
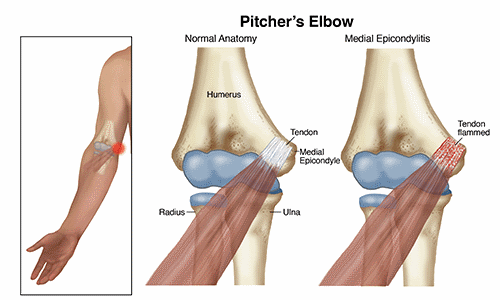
Pitcher's elbow (Medial Apophysitis)
Medial apophysitis, or pitcher's elbow, is a condition that occurs as a result of an injury or irritation to the inside of the elbow, commonly affecting young athletes. It is often classified as an "overuse syndrome" in baseball or softball players in the developmental stages of rapid growth (approximately 11 to 15 years of age). Pitcher’s elbowcan be identified and effectively treated by a physical therapist.
What is Medial Apophysitis?
Pitcher's elbow occurs when there is irritation to the inside portion of the elbow joint where the arm bone (humerus) meets one of the bones of the forearm (ulna).
During adolescence, the bones that form the elbow joint are still developing and are, therefore, more susceptible to injuries. During the throwing motion, stress is put on this part of the elbow. When too much stress is present (ie, from too much throwing) and when the joint is not able to recover properly (ie, when there is not enough rest time between periods of activity), the elbow can become painful and swollen. This results in the athlete being unable to throw with speed and accuracy at their normal volume. Pitcher's elbow can start as soreness, but if not diagnosed and treated early on, can progress to more serious injuries, such as tearing of the ligaments or fracture of the bone(s) of the joint.
How Does it Feel?
With pitcher's elbow, you may experience:
- Gradually worsening pain at the inside of your elbow when throwing a ball.
- Lingering soreness at the inside of your elbow following throwing activities.
- Swelling and tenderness around the inside area of the elbow area.
- Inability to throw the ball at your normal speed.
- Loss of grip strength.
- Loss of accuracy or distance when throwing.
- Muscle cramping in your forearm.
- Discomfort with daily activities that use your forearm muscles, like turning a doorknob or carrying a heavy object in front of you.
- Loss of motion of your elbow.
- Discomfort with daily activities that use your forearm muscles, like turning a doorknob or carrying a heavy object in front of you.
How Is It Diagnosed?
Diagnosis of pitcher's elbow begins with a thorough review of the athlete's medical history, including specific questions regarding athletic participation (sports played, frequency of practices and games, positions, types and numbers of pitches thrown). Your physical therapist will assess different measures, such as sensation, motion, strength, flexibility, tenderness, and swelling. The physical therapist will perform several tests specific to the elbow joint to examine the structures located there, and may ask you to briefly demonstrate the activities or positions that cause your pain. Depending on your symptoms, your physical therapist may even ask you to throw a baseball or softball to assess your throwing mechanics. The physical therapist will also ask you to give detailed information about your experience as a throwing athlete.
Because the shoulder and elbow are both involved in throwing, your physical therapist will likely examine your shoulder. Other nearby areas, such as your neck and upper back, will also be examined to determine whether they, too, might be contributing to your elbow condition.
If your physical therapist suspects there may be a more involved injury than overuse-related irritation (ie, if there is a recent significant loss of elbow motion or severe pain when the elbow is moved), the therapist may recommend a referral to an orthopedic physician for diagnostic imaging, such as ultrasound, x-ray, or MRI. All aspects of diagnosis, including subjective questioning, the clinical exam, and diagnostic imaging are important to determine the nature of your elbow injury.
How Can a Physical Therapist Help?
Once other conditions have been ruled out and pitcher’s elbow is diagnosed, your physical therapist will work with you to develop an individualized plan tailored to your specific elbow condition and your athletic goals. There are many physical therapy treatments that have been shown to be very effective in treating this condition. Your physical therapist may focus on:
Range of Motion. Because of the repetitive nature of throwing that causes the elbow to be irritated, it is often swollen and stiff, resulting in a loss of normal motion. You may also have abnormal motion of your throwing shoulder that is contributing to the way your elbow is acting during throwing. Your physical therapist will assess the motion of both of these joints compared to expected normal motion for your age and gender, as well as that of your other shoulder and elbow.
Strength Training. The muscles surrounding the shoulder and elbow as well as those of the upper back, work together to allow for normal, coordinated upper-body motion. This coordinated motion is especially important during throwing. Therefore, balancing the strength of all the upper-body muscles is crucial to making sure the shoulder and elbow joints move efficiently. Your physical therapist will teach you exercises to strengthen the muscles around the shoulder, so that each muscle is able to properly perform its job, and stresses are appropriately dispersed.
Manual Therapy. Physical therapists are trained in manual (hands-on) therapy. If needed, your physical therapist will gently move and mobilize your elbow and shoulder joint and surrounding muscles as needed to improve their motion, flexibility, and strength. These techniques can target areas that are difficult to treat on your own.
Pain Management. Your physical therapist may recommend therapeutic modalities, such as ice and heat to aid in pain management.
Functional Training. In the adolescent age group that typically suffers from pitcher’s elbow, an athlete is usually learning how to adapt their movements to a growing body. Poor coordination can place undue stress on the shoulder and elbow, and improper movements can, over time, cause pain in the body. Physical therapists are experts in assessing movement quality, and in training athletes to function at their best. Your physical therapist will point out and correct faulty movements in your throwing motion, so you are able to attain and maintain a pain-free elbow.
Education. The first step to addressing your elbow pain is rest. Your physical therapist will explain why this is so important, and develop a plan for your rehabilitation so you know when you will be able to safely return to your sport. Your physical therapist will also develop a personalized return-to-throwing progression of treatment and exercise, so you are able to move from your rest phase through a gradual reintegration of throwing activities to avoid another injury.
Can this Injury or Condition be Prevented?
Fortunately, there is much that can be done to prevent the cascade of events that lead to pitcher's elbow. Physical therapists help athletes and coaches focus on:
- Offering guidelines for throwing participation, explaining common causes of throwing-related injuries, and providing strategies for prevention.
- Educating athletes on the risks of playing through pain.
- Monitoring pitch counts, both during practice and game scenarios.
- Monitoring throwing participation (multiple sports, multiple leagues and teams, positions).
- Allowing adequate rest time for athletes to recover between throwing outings.
- Tracking a young athlete’s growth curves (height, weight, BMI).
- Developing an athlete-specific flexibility and strengthening routine that is done throughout the athletic season.
- Encouraging athletes to consult with a physical therapist if symptoms are worsening despite rest.
Cubital tunnel syndrome is the second most common nerve compression occurring in the arm. (Carpal tunnel syndrome is the most common.) It is a condition caused by increased pressure on the ulnar nerve at the elbow. This pressure can result in considerable discomfort and may progress to loss of function of the hand. Cubital tunnel syndrome generally affects men more than women, especially those with jobs that require repetitive elbow movements and prolonged elbow flexion. Symptoms can occur in both the dominant and the non-dominant arm.
Cubital tunnel syndrome is caused by compression of the ulnar nerve when it passes under a bony bump (medial epicondyle) on the inside portion of the elbow. In this area, the nerve is relatively unprotected and can be trapped between the bone and the skin in a tunnel called the cubital tunnel. Though it is not an actual bone, this area is commonly called your “funny bone.” When you hit the "funny bone" just the right way, you have actually hit the ulnar nerve. This contact sends a sensation of tingling, numbness and pain along the inside of your arm and down to the ring and little fingers. When the ulnar nerve is compressed, it causes the same type of symptoms. The ulnar nerve can be pinched at any point along its length, but the most common site of compression is on the cubital tunnel.
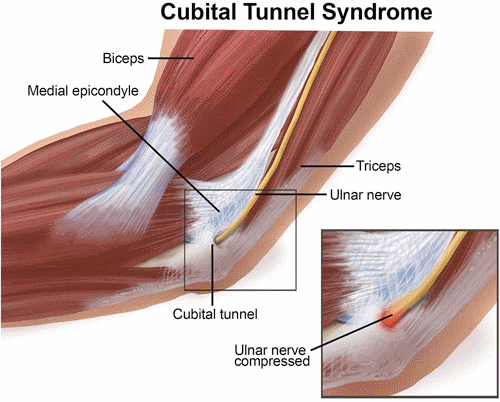
Cubital tunnel syndrome often results from prolonged stretch or pressure on the nerve. When the arm is bent for a long time, such as when holding the phone, it stretches the ulnar nerve across the inside of the elbow, creating a traction force that decreases the blood flow to the nerve and may cause nerve irritation. Prolonged pressure on the nerve may happen, for example, when the inside part of the elbow leans against a table and the ulnar nerve is pushed over the bone, which may cause the sensation of tingling, numbness and pain along the inside of your arm and hand.
Signs and Symptoms
Cubital tunnel syndrome can occur after a traumatic incident such as an elbow fracture, or it can develop slowly over time. It usually begins with numbness and/or tingling sensations (pins and needles) on the inside of the forearm extending down into the hand. Typical symptoms include:
- Intermittent pain or numbness and tingling brought on by sustained bending of the elbow over a long period of time
- Tenderness on the inside of the elbow where the nerve is close to the surface
- Decreased sensation or difficulty telling the difference between sharp and dull objects touching the inside of the forearm
Later symptoms sometimes include:
- Difficulty gripping and holding on to objects (clumsy hands)
- Muscle wasting of the small muscles of the hand
- A hand deformity in which the fingers bend inward, referred to as an "ulnar claw hand"
How Is It Diagnosed?
Cubital tunnel syndrome can be diagnosed by a physical therapist or a physician. Your physical therapist will typically perform a comprehensive evaluation that may include assessment of your neck to rule out compression of the nerve where it starts in the neck. After determining that the nerve being compressed is truly the ulnar nerve, your physical therapist will use tests that may include:
- Observation and inspection of the elbow and forearm
- Touching and moving the arm in the area of the nerve to determine its relationship to the elbow and its stability in the groove behind the elbow where the nerve travels
- Tapping the nerve at the elbow (the Tinel's sign test)
- A sensory examination that includes both light touch and a test of the ability to distinguish between sharp or dull stimulus and temperature
- Checking the strength of specific muscles of your hand
- Checking your pinching and gripping ability
Cubital tunnel syndrome can be accurately diagnosed clinically without additional testing. Occasionally you may be referred for electrodiagnostic tests called electromyography (EMG) and/or nerve conduction study (NCS). These tests evaluate the ability of the nerve to conduct signals along its full length. They can help determine the exact site of the compression and estimate the extent of the compression.
How Can a Physical Therapist Help?
Many cases of cubital tunnel syndrome can be treated without surgery. Your physical therapist will determine the activities that bring on your symptoms. The recommendations at this point will be to avoid those activities for a time. Remember, the nerve is irritated and at times swollen. If the irritation and swelling can be reduced, the symptoms should resolve.
In more advanced cases, your physical therapist will modify your activity and may recommend you use a splint to take the pressure off of the nerve. As your condition begins to improve, your therapist may teach you:
- Range-of-motion exercises to help return full length to the muscles that have shortened due to protective posturing, and to maintain the normal length of those that have remained unaffected.
- Muscle strengthening exercises to help restore the strength that has been lost over time. Your therapist will help pick the exercises that are right for you.
- "Nerve gliding" exercises. Nerves actually have the ability to “stretch out.” Your therapist is educated in the proper positions for appropriate nerve stretches, and will work with you to ensure that safe and gentle stretching is achieved. In cubital tunnel syndrome, the nerve can become shortened; these exercises are an effective means of returning the nerve to its normal length.
Sometimes surgery is required. The longer you have experienced symptoms and the more you experience weakness, numbness, tingling, and pain the more likely you are to need surgery. The goal of surgery is to relieve the pressure on the nerve.
Your physical therapist will design an individual program of post-surgical therapy based on the operation and the surgeon’s instructions. Each surgery will require a unique treatment regimen, but the post-surgical rehabilitation will involve many of the pre-surgical elements discussed above, with the exclusion of nerve gliding exercises. Activity modification will be a big part of your post-surgical rehabilitation to prevent recurrence of your symptoms.
Can this Injury or Condition be Prevented?
Little is known about prevention of cubital tunnel syndrome. Often, the syndrome is not diagnosed until symptoms are already present. However, some general precautions may be taken.
- Obesity has been linked by some researchers to cubital tunnel syndrome. Healthy lifestyle choices and a reduction in your weight may help prevent its development.
- People in occupations that require holding the elbow in a bent position should be encouraged to perform consistent positional changes to take stress off of the ulnar nerve.
- Diabetes has been recognized as a risk factor.
- Recommendations for activity modification can sometimes be disruptive to employment, but they have been shown to have the most significant positive response when treating cubital tunnel syndrome non-surgically.
