-
 Injury keeping you out of the game?Our experts will get to the core of your fitness needs.OUR SERVICES
Injury keeping you out of the game?Our experts will get to the core of your fitness needs.OUR SERVICES -
 GET BACK TO THE ACTIVITIES YOU LOVEOUR SERVICES
GET BACK TO THE ACTIVITIES YOU LOVEOUR SERVICES -
 RESTORING YOUR PHYSICAL ABILITYOUR SERVICES
RESTORING YOUR PHYSICAL ABILITYOUR SERVICES -
 RESTORING YOUR QUALITY OF LIFEOUR SERVICES
RESTORING YOUR QUALITY OF LIFEOUR SERVICES -
 EVIDENCE BASED PRACTICEOUR SERVICES
EVIDENCE BASED PRACTICEOUR SERVICES -
 APPROPRIATE PROGRAM FOR A SUCCESSFUL RECOVERYOUR SERVICES
APPROPRIATE PROGRAM FOR A SUCCESSFUL RECOVERYOUR SERVICES -
 HELPING YOU ACHIEVE YOUR GOALSOUR SERVICES
HELPING YOU ACHIEVE YOUR GOALSOUR SERVICES
Hip
Pelvic Fracture (Hip Fracture)
A pelvic fracture is a crack or break in one or more of the pelvic bones, which are located at the base of the spine. The pelvis is often referred to as part of the hip. (When you "put your hands on your hips," your hands are actually resting on your pelvic bones.) Pelvic fractures in the United States are relatively rare, making up 0.3% to 6% of all fractures. Pelvic fractures are most common in people 15-28 years of age. In people younger than 35, males suffer a higher incidence of pelvic fractures than females. In people older than 35, females suffer pelvic fractures more often than males.
A pelvic fracture can result from a low-impact or high-impact event.
Low-impact pelvic fractures most commonly occur in 2 age groups: adolescents and the elderly. Adolescents typically experience fractures of the tips of 1 of the pelvic bones, resulting from an athletic injury (football, hockey, skiing) or an activity such as jogging. Pelvic fractures also can occur after minor falls in people with osteoporosis or even occur spontaneously when bones are weak. The elderly frequently suffer fractures of the thicker part of the pelvic bones. These "pelvic ring fractures" result from falling onto the side of the hip. These falls can be caused by balance problems, vision problems, medication side effects, general frailty, or unintended obstacles such as pets underfoot, slippery floors, or rumpled rugs. Low-impact pelvic fractures often are mild fractures, and they may heal with several weeks of rest. Physical therapy is very helpful in restoring strength and balance in these cases.
High-impact pelvic fractures most commonly result from major incidents such as a motor vehicle accidents, a pedestrian being struck by a vehicle, or a fall from a high place. These pelvic fractures can be life-threatening, require emergency room care, surgery, and extensive physical therapy rehabilitation.
A pelvic fracture is a break in 1 or more bones in the pelvis. It is sometimes referred to as a "hip fracture" or "broken hip" because it occurs in the bones that make up the hip area. A pelvic fracture causes difficulty walking or standing. It can also cause abdominal pain, bleeding from pelvic cavities, and difficulty urinating.
How Can a Physical Therapist Help?
Pelvic fracture recovery often involves surgery or long periods of bed rest. In the case of athletes, avoidance of sport activities is recommended until pain has resolved. During these periods of rest, which are usually weeks to months, a person often loses strength, flexibility, endurance, and balance abilities.
Physical therapists can help you recover from a pelvic fracture by improving your:
- Pain level
- Hip, spine, and leg motion
- Strength
- Flexibility
- Speed of healing
- Speed of return to activity and sport
When you are cleared by your physician to begin physical therapy, your physical therapist will design a specific treatment program to speed your recovery, including exercises and treatments you should do at home. This program will help you return to your normal life and activities and reach your recovery goals.
The First 24-48 Hours
Your physical therapist may help you learn to use crutches so you can move around your home without walking on the leg of the injured side. This will more commonly apply to low-impact pelvic fractures, as in athletes. More severe pelvic fractures will require a wheelchair, in which your physical therapist can instruct your safe usage.
Reduce Pain
Your physical therapist can use different types of treatments and technologies to control and reduce your pain, including ice, heat, ultrasound, electrical stimulation, taping, exercises, and special hands-on techniques called manual therapy that gently move your muscles and joints.
Your physical therapist will choose specific activities and treatments to help restore normal movement in the leg and hip. These might start with passive motions that he or she applies to your leg and hip joint, and progress to active exercises and stretches that you perform yourself. Treatment can involve hands-on manual therapy techniques called "trigger point release" and "soft tissue mobilization," as well as specific stretches to muscles that might be abnormally tight.
Improve Strength
Certain exercises will benefit your healing at each stage of recovery, and your physical therapist will choose and teach you an individualized exercise program that will restore your strength, power, and agility. These exercises may be performed using free weights, stretch bands, weight-lifting equipment, and cardio exercise machines such as treadmills and stationary bicycles. For pelvic fractures, muscles of the hip and core are often targeted by the strength exercises.
Improve Balance
The hip area contains many muscles that are vital for balance and steadiness when walking or p
Speed Recovery Time
Your physical therapist is trained and experienced in choosing the treatments and exercises to help you heal, get back to your normal life, and reach your goals faster than you might be able to on your own.
Return to Activities
Your physical therapist will collaborate with you to decide on your recovery goals, including return to work and sport. Your treatment program will be designed to help you reach these goals in the safest, fastest, and most effective way possible. Your physical therapist will use hands-on therapy and teach you exercises and work re-training activities. Athletes will be taught sport-specific techniques and drills to help achieve sports-specific goals.
Prevent Future Problems
Your physical therapist can recommend a home exercise program to strengthen and stretch the muscles around your hip, upper leg, and core to help prevent future problems, such as fatigue and walking difficulty. This program may include strength and flexibility exercises for the hip, thigh, and core muscles. Your physical therapist will also review with you and your family ways to prevent falls in your home. These fall-prevention strategies may include clearing the floors of loose obstacles (throw rugs, mats), using sticky mats or chairs in the shower, preventing pets from walking near your feet, and using non-slippery house shoes, as well as installing grab bars or rails for the shower, toilet, and stairs.
If Surgery Is Necessary
If surgery is required, your physical therapist will help you minimize pain, restore motion and strength, and return to normal activities in the speediest manner possible after surgery.
Can this Injury or Condition be Prevented?
Pelvic fracture can be prevented by:
- Warming up before starting any sport or heavy physical activity. Your warm-up should include stretches taught to you by your physical therapist, including stretches for the muscles on the front, side, and back of the hip.
- Increasing the intensity of an activity or sport gradually, not suddenly. Avoid pushing yourself too hard, too fast, too soon.
- Following a reasonable and safe nutritional plan. Nutritional factors can contribute to osteoporosis, which can put you at higher risk of pelvic fracture.
- Maintaining good balance skills. Balance problems can increase the risk of falling and thus increase the risk of incurring a pelvic fracture. Physical therapy can help maintain and improve balance ability, which can help prevent falls.
- Driving safely to avoid motor vehicle accidents.
- Clearing your house of obstacles that you could trip over, and eliminating slippery walking surfaces.
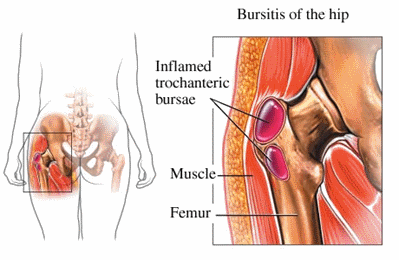
Hip bursitis is a painful condition that affects 15% of women and 8.5% of men of all ages in the United States. The condition tends to develop more in middle-aged and elderly individuals. Hip bursitis can have many causes, but the most common is a repetitive activity, such as walking or running on an uneven surface, which creates friction in the hip area. Athletes often develop hip bursitis after running up and down hills repetitively. The condition can also be caused by abnormal walking, such as limping, due to an uneven leg length, or arthritis in the back, hip, knee, or other joints in the leg. It can also occur without any specific cause. Physical therapy can be an effective treatment for hip bursitis to reduce pain, swelling, stiffness, and any associated weakness in the hip, back, or lower extremity.
What is Hip Bursitis?
Hip bursitis (also called trochanteric bursitis) occurs when one or both of the 2 bursae (fluid-filled sacs on the side of the hip) become damaged, irritated, or inflamed. Bursitis (“-itis” means “inflammation of”) means the bursa has become irritated and inflamed, usually causing pain. Normally, the bursa acts as a cushion for muscles and tendons that are close to it. Certain positions, motions, or disease processes can cause constant friction or stress on the bursa, leading to the development of bursitis. When the bursa becomes injured, those muscles and tendons don’t glide smoothly over it, and they can become painful.
Hip bursitis can be caused by:
- Repetitive motions (running up and down hills or stairs)
- Muscle weakness
- Incorrect posture
- Direct trauma (being hit or falling on the side of the hip)
- Differences in the length of each leg
- Hip surgery or replacement
- Bone spurs in the hip
- Infection
- Diseases, such as rheumatoid arthritis, gout, psoriasis, or thyroid disease
- Muscles or tendons in the hip area rubbing the bursa and causing irritation
How Does it Feel?
With hip bursitis, you may experience:
- Pain on the outer side of the hip, thigh, buttock, or outside of the leg.
- Pain when you push on the outer side of the hip with your fingers.
- Pain when lying on the affected hip.
- Pain when climbing stairs.
- Pain that worsens when getting up from sitting, such as from a low chair or car seat.
- Pain when walking or running.
- Pain when lifting the leg up to the side.
- Pain when sitting with legs crossed.
How Is It Diagnosed?
If you see your physical therapist first, the physical therapist will conduct a thorough evaluation that includes taking your health history. Your physical therapist also will ask you detailed questions about your condition, such as:
- How and when did you notice the pain?
- Have you been performing any repetitive activity?
- Did you receive a direct hit to the hip or fall on it?
Your physical therapist will perform special tests to help determine the likelihood that you have hip bursitis. Your physical therapist will gently press on the outer side of the hip to see if it is painful to the touch, and may use additional tests to determine if other parts of your hip are injured. Your physical therapist also will observe how you are walking.
Your physical therapist will test and screen for other, more serious conditions that could cause lateral hip pain. To provide a definitive diagnosis, your physical therapist may collaborate with an orthopedic physician or other health care provider, who may order further tests (eg, an x-ray) to confirm the diagnosis and rule out other damage to the hip, such as a fracture.
How Can a Physical Therapist Help?
Your physical therapist will work with you to design a specific treatment program that will speed your recovery, including exercises and treatments that you can do at home. Physical therapy will help you return to your normal lifestyle and activities. The time it takes to heal the condition varies, but results can be achieved in 2 to 8 weeks or less, when a proper stretching and strengthening program is implemented.
During the first 24 to 48 hours following your diagnosis, your physical therapist may advise you to:
- Rest the area by avoiding walking or any activity that causes pain.
- Apply ice packs to the area for 15 to 20 minutes every 2 hours.
- Consult with a physician for further services, such as medication or diagnostic tests.
Your physical therapist will work with you to:
Reduce Pain and Swelling. If repetitive activities have caused the hip bursitis, your physical therapist will help you understand how to avoid or modify your activities to allow healing to begin. Your physical therapist may use different types of treatments and technologies to control and reduce your pain and swelling, including ice, heat, ultrasound, electrical stimulation, taping, exercises, and hands-on therapy, such as specialized massage.
Improve Motion. Your physical therapist will choose specific activities and treatments to help restore normal movement in the hip and leg. These might begin with "passive" motions that the physical therapist performs for you to gently move your hip joint, and progress to active exercises and stretches that you do yourself.
Improve Flexibility. Your physical therapist will determine if any leg or spinal muscles are tight, help you to stretch them, and teach you how to stretch them.
Improve Strength. Hip bursitis is often related to weak or injured hip muscles. Certain exercises will aid healing at each stage of recovery; your physical therapist will choose and teach you the correct exercises and equipment to steadily restore your strength and agility. These may include using cuff weights, stretch bands, weight-lifting equipment, and cardio-exercise equipment, such as treadmills or stationary bicycles.
Improve Balance. Regaining your sense of balance is important after an injury. Your physical therapist will teach you exercises to improve your balance skills.
Learn a Home-Exercise Program. Your physical therapist will teach you strengthening and stretching exercises to perform at home. These exercises will be specific for your needs; if you do them as prescribed by your physical therapist, you can speed your recovery.
Return to Activities. Your physical therapist will discuss your activity goals with you and use them to set your work, sport, and home-life recovery goals. Your treatment program will help you reach your goals in the safest, fastest, and most effective way possible. Your physical therapist will teach you exercises, work retraining activities, and sport-specific techniques and drills that match your lifestyle.
Speed Recovery Time. Your physical therapist is trained and experienced in choosing the best treatments and exercises to help you safely heal, return to your normal lifestyle, and reach your goals faster than you are likely to do on your own.
If Surgery Is Necessary
Surgery is not commonly required for hip bursitis. However, if surgery is needed, you will follow a recovery program over several weeks guided by your physical therapist. Your physical therapist will help you minimize pain, regain motion and strength, and return to normal activities in the safest and speediest manner possible.
Can this Injury or Condition be Prevented?
Your physical therapist can recommend a home-exercise program to strengthen and stretch the muscles around your knee, upper leg, and abdomen to help prevent future injury. These may include strength and flexibility exercises for the leg, knee, and core muscles.
To help prevent a recurrence of the injury, your physical therapist may advise you to:
- Follow a consistent flexibility and strengthening exercise program, especially for the hip muscles, to maintain good physical conditioning, even in a sport's off-season.
- Always warm up before starting a sport or heavy physical activity.
- Gradually increase any athletic activity, rather than suddenly increasing the activity amount or intensity.
- Obtain a professionally fitted shoe insert, if your legs are different lengths.
- Learn and maintain correct posture.
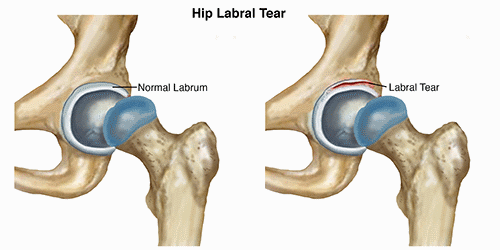
Hip labral tears occur when the labrum, a band of cartilage surrounding the hip joint, is injured. Labral injuries can be the result of trauma, such as a fall or a car accident, but are most commonly caused by repetitive trauma to the hip joint. Individuals who participate in sports that require extremes of motion, such as figure skating, repetitive twisting and "cutting," like hockey or soccer, or long-distance running are most often diagnosed with labral tears. To treat the symptoms associated with a labral tear, physical therapists typically prescribe a combination of stretching and strengthening activities to decrease irritation in the hip.
What is a Hip Labral Tear?
A hip labral tear occurs where there is damage to the labrum within the hip joint. The hip joint is where the thigh bone (femur) meets the pelvis (Ilium). It is described as a ball-and-socket joint. This design allows the hip to move in several directions. The bony socket is surrounded by a ring of cartilage called the labrum. The labrum provides additional stability to the hip joint.
A labral tear results when a part of the labrum separates or is pulled away from the socket. Most often, a labral tear is the result of repetitive trauma to the hip, either due to running or repeated twisting and cutting
Hip labral tears may result from a combination of several different variables, including:
- Bony abnormalities in the hip joint (hip impingement)
- Hip muscle tightness
- Hip muscle weakness
- Improper technique with repetitive activities
- Participation in sports that require distance running, or repetitive twisting and cutting
Once torn, the labral tissue in the hip does not have the ability to heal on its own. There are surgical procedures to remove or repair torn labral tissue; however, treatment for a labral tear often begins with a course of physical therapy.
Nonsurgical treatment efforts are focused on addressing symptoms by maximizing the strength and mobility of the hip to minimizing the stress placed on the injured area. In certain cases, patients are able to achieve a satisfactory level of activity without surgery.
Surgical interventions are available to clean out the hip joint, and repair or reconstruct the torn labral tissue. Following surgery, patients will complete several months of physical therapy to regain function of the hip.
How Does it Feel?
Pain in the front of the hip or in the groin resulting from a hip labral tear, can cause an individual to have limited ability to stand, walk, climb stairs, squat, or participate in recreational activities. You may experience:
- A deep ache in the front of your hip or groin, often described by the "C sign." (People make a "C" with the thumb and hand, and place it on the fold at the front and side of the hip to locate their pain.)
- Painful clicking or "catching" with hip movements. This creates the feeling of something painful stuck in the hip or blocking hip motion.
- Pain that increases with prolonged sitting or walking.
- A sharp pain in the hip or groin when squatting.
- Pain that comes on gradually rather than with 1 specific episode.
- Weakness in the muscles surrounding the hip.
- Stiffness in the hip.
How Is It Diagnosed?
Your physical therapist will review your medical history and complete a thorough examination of your hip, and possibly your lower back and knee. The goals of the initial examination are to assess the degree of the injury, and determine the cause and contributing factors to it. A hip labral tear may be the result of a single injury, but most likely is a condition that develops as a consequence of repetitive irritation in the hip.
Your physical therapist will assess the mobility and strength of your hip, and may watch you walk, step onto a stair, squat, or balance on 1 leg. Your physical therapist will also gently touch the front, side, and back of your hip to determine exactly where it is most painful.
Your physical therapist may also ask questions regarding your daily activities—most importantly, activities that aggravate and relieve your symptoms. Your physical therapist will also ask about your exercise regimens and footwear, to identify other possible contributing factors to your pain.
Your physical therapist may also refer you to an orthopedic physician who specializes in hip injuries for diagnostic imaging (i.e., x-ray, MRI). An x-ray helps to identify any bony abnormalities, such as hip impingement that may be contributing to your pain. An MRI helps to identify a labral tear.
How Can a Physical Therapist Help?
When you have been diagnosed with a hip labral tear, your physical therapist will work with you to develop a plan to help achieve your specific goals. To do so, your physical therapist will select treatment strategies in any or all of the following areas:
- Pain management. Many pain-relief strategies may be implemented; the most beneficial with hip pain is to apply ice to the area and decrease or eliminate specific activities for a certain length of time. Your physical therapist will help to identify specific movements or activities that continue to aggravate the inside of your hip joint. Your physical therapist then will design an individual treatment plan for you, beginning with a period of rest, and gradually adding a return to certain activities as appropriate.
- Movement re-education. Your back and hip may be moving improperly, causing increased tension at the hip joint. Self-stretching techniques may be applied to the lower body to decrease tension and help restore normal motion in the back, hip, and leg. There are, however, certain hip motions to avoid following an injury to the hip labrum. Your physical therapist will carefully prescribe exercises that improve your range of motion, while protecting the area that has the labral tear.
- Manual therapy. Your therapist may apply hands-on treatments to gently move your muscles and joints to decrease your pain and improve motion and strength. These techniques often address areas that are difficult to treat on your own.
- Muscle strengthening. Muscular weaknesses or imbalances can be the cause or the result of hip pain. Based on your specific condition, your physical therapist will design a safe, individualized, progressive resistance program for you, likely including your core (midsection) and lower extremity. You may begin by performing strengthening exercises lying on a table, for example, lifting your leg up while lying in different positions. You then may advance to doing exercises in a standing position, for example, stepping on and off a raised platform. Your physical therapist will choose what exercises are right for you.
- Functional training. Once your pain, strength, and motion improve, you will be able to safely transition back into more demanding activities. To minimize tension on the hip, it is important to teach your body safe, controlled movements. Based on your own unique movement assessment and goals, your physical therapist will create a series of activities to help you learn how to use and move your body correctly and safely. Your physical therapist will also discuss specific positions and activities that should be avoided or modified to protect your hip.
- Education. Your physical therapist will work with you to identify and change any external factors causing your pain, such as exercise selection, footwear, or the amount of exercises you complete. Your physical therapist will develop a personal exercise program to help you return to your desired activities.
Can this Injury or Condition be Prevented?
Maintaining appropriate lower-extremity mobility and muscular strength are the best methods for preventing a hip labral tear.
Unfortunately, the way the hip and pelvis bones of some individuals are structured, the risk of sustaining a labral injury can increase. It is imperative to be aware of any hip pain that you experience, particularly with sitting and squatting, as these are signs of a potential hip injury. Identifying and addressing these injuries early is helpful in their treatment.
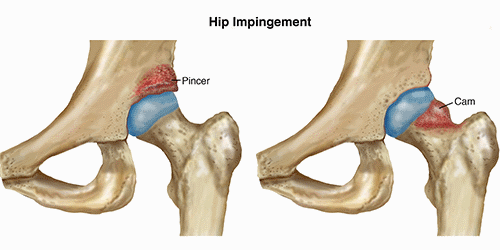
Hip impingement involves a change in the shape of the surface of the hip joint that predisposes it to damage, resulting in stiffness and pain. Hip impingement is a process that may precede hip osteoarthritis. It most often occurs in young, active people. A recent study found that 87% of teens and adults with hip pain showed evidence of hip impingement on diagnostic images taken of their hip joints. To treat hip impingement, physical therapists prescribe stretches and strengthening exercises to better balance the muscles around the hip to protect it, and use manual therapies to help restore range of motion and increase comfort.
There are 2 types of hip impingement; they may occur alone or together.
Pincer-Type Impingement
- In pincer-type impingement, the hip socket (acetabulum), which is usually angled forward, may be angled toward the back, or protruding bone may be present on the pelvis side of the hip joint making the socket a deeper recess that covers more of the ball or head of the femur bone.
- The overgrown bone or incorrect angle of the socket causes the labrum, a rim of connective tissue around the edge of the hip socket, to be pinched. Over time, this extra pressure to the labrum when flexing (moving the leg forward) leads to wear and tear that can cause inflammation and could result in a tear. If this condition persists, eventually the cartilage that lines the hip joint can become worn and form holes.
- This condition affects men and women equally; symptoms often begin early, appearing at any time between 15 to 50 years of age.
Cam-Type Impingement
- In cam-type impingement, the shape of the bone around the head of the femur—the ball at the top of the bone in the thigh—is misshapen. It can vary from the normal round ball shape, or have overgrown bone formed at the top and front. The nickname “pistol grip” deformity is given to the appearance of the bony overgrowth on x-rays.
- The overgrown or misshapen bone contacts the cartilage that lines the hip socket, and can cause it to peel away from the bone in the socket. The labrum can become worn, frayed, or torn as well.
- This condition affects men to women at a ratio of 3 to 1; symptoms often manifest during the teen years and 20s.
Signs and Symptoms
Hip impingement may cause you to experience:
- Stiffness or deep aching pain in the front or side of the hip or front of the upper thigh while resting.
- Sharp, stabbing pain when standing up from a chair, squatting, rising from a squat, running, "cutting," jumping, twisting, pivoting, or making lateral motions.
- Hip pain described in a specific location by making a "C" with the thumb and hand and placing it on the fold at the front and side of the hip, known as the "C-sign."
- Pain that most often starts gradually, but can also remain after another injury resolves.
- Pain that increases with prolonged sitting or forward leaning.
- Feeling less flexible at the hips, including a decreased ability to turn your thigh inward on the painful side.
How Is It Diagnosed?
Your physical therapist will evaluate the range of motion (movement) of the hip and surrounding joints, and test the strength of the muscles in that area. Your therapist will feel the hip joint and surrounding muscles to evaluate their condition. The examination will include observing how you move, standing from a sitting position, walking, running, or squatting, as appropriate. Your physical therapist may perform special tests to help determine whether the hip is the source of your symptoms. For instance, the therapist may gently roll your leg in and out (the “log roll” test), or bend your hip up and in while turning the lower leg out to the side (the "FADDIR" test) to assess your condition.
If further diagnosis is needed, your doctor may order diagnostic tests to help identify any joint changes, including x-rays, magnetic resonance imaging (MRI), or diagnostic injections. Hip impingement can occur at the same time as low back, buttock, or pelvic pain, or from conditions such as bursitis or groin strain. The final diagnosis of hip impingement may take some time, especially when other conditions are present.
How Can a Physical Therapist Help?
Without Surgery
When an active person develops hip pain, but does not have severe symptoms or joint damage, the recommended treatment is physical therapy. The following interventions can help decrease pain, improve movement, and avoid the progression of hip impingement and the need for surgery:
- Improving the strength of your hips and trunk. Strengthening of the hips and trunk can reduce abnormal forces on the already injured joint and help with strategies to compensate.
- Improving hip muscle flexibility and joint mobility. Stretching tight muscles can reduce abnormal forces that cause pain with motion. Joint mobilization may help ease pain from the hip joint; however, these treatments do not always help range of motion, especially if the shape of the bone at the hip joint has changed.
- Improving tolerance of daily activities. Your physical therapist can consider your job and recreational activities and offer advice regarding maintaining postures that are healthier for your hip and activity modification. Often this involves limiting the amount of bending at the hip to avoid further hip damage.
Following Surgery
Surgery for hip impingement is performed with arthroscopy. This is a minimally invasive type of surgery, where the surgeon makes small incisions in the skin and inserts pencil-sized instruments into the joint to repair damage. The surgeon may perform 1 or several techniques during your procedure as needed. The surgeon may remove or reshape the bone on the pelvis or femur side of the joint, and repair or remove the damaged labrum or cartilage of the hip joint.
Postsurgical physical therapy varies based on the procedure performed. It may include:
- Ensuring your safety as you heal. Your physical therapist may recommend that you limit the amount of weight you put on the operated leg if there was a repair of the labrum. You may wear a brace to help limit the amount of bending at the hip. You might also use crutches to avoid overloading the leg if the bone on the femur was reshaped.
- Improving your range of motion, strength, and balance. Your physical therapist will guide you through safe range-of-motion, strengthening, and balance activities to improve your movement as quickly as possible while allowing the surgical site to heal properly.
- Instructions on returning to an active lifestyle. Most people return to normal daily activities about 3 months after surgery, and to high-level activities and sports 4 to 6 months after surgery. Your physical therapist will recommend a gradual return to activity based on your condition—research shows that 60% to 90% of athletes return to their previous playing ability depending on the surgical procedure performed and the sport.
Can this Injury or Condition be Prevented?
Currently there are no recommendations to prevent hip impingement. Despite a major increase in research to learn more about hip impingement, there is a great deal that is unknown. For instance, many active young people whose x-rays show hips as being abnormal do not have pain despite continuing to live active lives and participate in sports.
However, there is evidence that physical therapy interventions along with anti-inflammatory drugs can decrease pain, slow joint damage, and improve function. This is particularly important in those with mild hip impingement, those who are attempting to avoid surgery, and those who are not candidates for surgery.
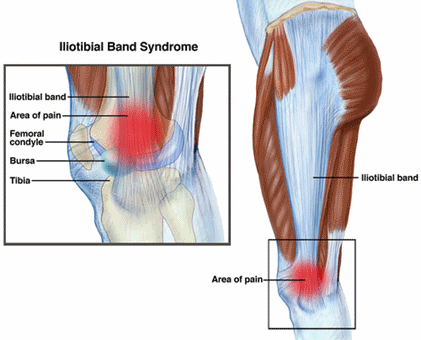
Iliotibial band syndrome (ITBS) is one of the most common causes of knee pain, particularly in individuals involved in endurance sports. It accounts for up to 12% of running injuries and up to 24% of cycling injuries. ITBS is typically managed conservatively through physical therapy and temporary activity modification.
What is Iliotibial Band Syndrome (ITBS)?
Iliotibial band syndrome (ITBS) occurs when excessive irritation causes pain at the outside (or lateral) part of the knee. The iliotibial band (ITB), often referred to as the "IT band" is a type of soft tissue that runs along the side of the thigh from the pelvis to the knee. As it approaches the knee, its shape thickens as it crosses a prominent area of the thigh (femur) bone, called the lateral femoral condyle. Near the pelvis, it attaches to 2 important hip muscles, the tensor fascia latae (TFL) and the gluteus maximus.
Irritation and inflammation arise from friction between the ITB and underlying structures when an individual moves through repetitive straightening (extension) and bending (flexion) of the knee. Typically, ITBS pain occurs with overuse during activities such as running and cycling.
ITBS involves many lower extremity structures, including muscles, bones, and other soft tissues. Usually discomfort arises from:
- Abnormal contact between the ITB and thigh (femur) bone
- Poor alignment and/or muscular control of the lower body
- Prolonged pinching (compression) or rubbing (shearing) forces during repetitive activities
The common structures involved in ITBS are:
- Iliotibial band
- Bursa (fluid-filled sack that sits between bones and soft tissues to limit friction)
- Hip muscles
ITBS can occur in:
- Athletes performing repetitive activities, such as squatting, and endurance sports such as running and cycling
- Individuals who spend long periods of time in prolonged positions, such as sitting or standing for a long workday, climbing or squatting, or kneeling
- Individuals who quickly start a new exercise regimen without proper warm-up or preparation
Signs and Symptoms
With ITBS, you may experience:
- Stabbing or stinging pain along the outside of the knee
- A feeling of the ITB “snapping” over the knee as it bends and straightens
- Swelling near the outside of your knee
- Occasionally, tightness and pain at the outside of the hip
- Continuous pain following activity, particularly with walking, climbing, or descending stairs, or moving from a sitting to standing position
Pain is usually most intense when the knee is in a slightly bent position, either right before or right after the foot strikes the ground. This is the point where the ITB rubs the most over the femur.
How Is It Diagnosed?
Your physical therapist will ask you questions about your medical history and activity regimen. A physical examination will be performed so that your physical therapist can collect movement (range of motion), strength, and flexibility measurements at the hip, knee, and ankle.
When dealing with ITBS, it is also common for a physical therapist to use special tests and complete a movement analysis, which will provide information on the way that you move and how it might contribute to your injury. This could include assessment of walking/running mechanics, foot structure, and balance. Your therapist may have you repeat the activity that causes your pain to see firsthand how your body moves when you feel pain. If you are an athlete, your therapist might also ask you about your chosen sport, shoes, training routes, and exercise routine.
Typically, medical imaging tests, such as x-ray and MRI, are not needed to diagnosis ITBS.
How Can a Physical Therapist Help?
Your physical therapist will use treatment strategies to focus on:
Range of motion
Often, abnormal motion of the hip and knee and foot joint can cause ITBS because of how the band attaches to hip muscles. Your therapist will assess the motion of your injury leg compared with expected normal motion and the motion of the hip on your uninvolved leg.
Muscle strength
Hip and core weakness can contribute to ITBS. The "core" refers to the muscles of the abdomen, low back, and pelvis. Core strength is important, as a strong midsection will allow greater stability through the body as the arms and legs go through various motions. For athletes performing endurance sports, it is important to have a strong core to stabilize the hip and knee joints during repetitive leg motions. Your physical therapist will be able to determine which muscles are weak and provide specific exercises to target these areas.
Manual therapy
Many physical therapists are trained in manual therapy, which means they use their hands to move and manipulate muscles and joints to improve motion and strength. These techniques can target areas that are difficult to treat on your own.
Functional training
Even when an individual has normal motion and strength, it is important to teach the body how to perform controlled and coordinated movements so there is no longer excessive stress at the previously injured structures. Your physical therapist will develop a functional training program specific to your desired activity. This means creating exercises that will replicate your activities and challenge your body to learn the correct way to move.
Your physical therapist will also work with you to develop an individualized treatment program specific to your personal goals. He or she will offer tips to help you prevent your injury from reoccurring.
Can this Injury or Condition be Prevented?
Maintaining core and lower extremity strength and flexibility and monitoring your activity best prevents ITBS. It is important to modify your activity and contact your physical therapist soon after first feeling pain. Research indicates that when soft tissues are irritated and the offending activity is continued, the body does not have time to repair the injured area. This often leads to persistent pain, and the condition becomes more difficult to resolve.
Once you are involved in a rehabilitation program, your physical therapist will help you determine when you are ready to progress back to your previous activity level. He or she will make sure that your body is ready to handle the demands of your activities so that your injury does not return. You will also receive a program to perform at home that will help you maintain the improvements that you gained during rehabilitation.
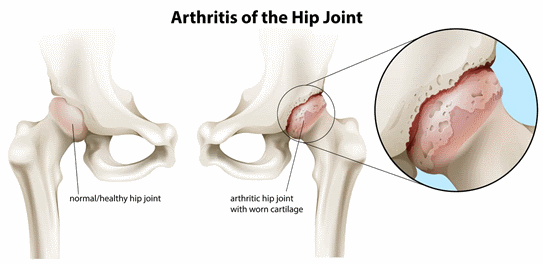
Hip osteoarthritis is inflammation of the hip joint. It can develop at any age, although it is more commonly diagnosed in older adults. Hip osteoarthritis can make everyday activities such as walking or climbing stairs difficult.
The Centers for Disease Control and Prevention reports that 25% of all people may develop painful hip osteoarthritis by age 85. There is no known specific cause of the condition; everyone is at equal risk of developing it. Recent research found no difference in the rate of occurrence of hip osteoarthritis in the general public based on race, gender, weight, or educational level.
Hip osteoarthritis is inflammation of the hip joint, a condition that is more likely to develop as people age. Osteoarthritis results when injury or inflammation in a joint causes the soft, shock-absorbing cartilage that lines and cushions the joint surfaces to break down. When the cartilage is damaged, the joint can become painful and swollen. Over time, this condition can cause stiffness and more pain.
How Does it Feel?
Hip osteoarthritis may cause:
- Sharp, shooting pain or dull, achy pain in the hip, groin, thigh, knee, or buttocks
- Stiffness in the hip joint, which is worse after sleeping or sitting
- A "crunching"; sound when the hip joint is moved, caused by bone rubbing on bone
- Difficulty and pain when getting out of bed, standing up from a sitting position, walking, or climbing stairs
- Difficulty performing normal daily activities, such as putting on socks and shoes
How Is It Diagnosed?
If you see your physical therapist first, the therapist will conduct a full evaluation that includes your medical history, and will ask you questions such as:
- When and how frequently do you feel pain and/or stiffness?
- What activities in your life are made difficult by this pain and stiffness?
He or she will perform special tests to help determine whether you have hip osteoarthritis, such as:
- Gently moving your leg in all directions (range of motion test)
- Asking you to resist against her hand as she tries to gently push your leg and hip in different directions (muscle strength test)
- Watching you walk to check for limping
- Asking you to balance while standing (balance test)
Your physical therapist may use additional tests to look for problems in other parts of your body, such as your lower back. He or she may recommend that you consult with an orthopedist, who can order diagnostic testing such as an x-ray or MRI, to confirm the diagnosis.
How Can a Physical Therapist Help?
Your physical therapist will explain what hip osteoarthritis is, how it is treated, the benefits of exercise, the importance of increasing overall daily physical activity, and how to protect the hip joint while walking, sitting, stair climbing, standing, load carrying, and lying in bed.
Testing will reveal any specific physical problems you have that are related to hip osteoarthritis, such as loss of motion, muscle weakness, or balance problems.
The pain of hip osteoarthritis can be reduced through simple, safe, and effective physical activities such as walking, riding a bike, or swimming.
Although physical activity can delay the onset of disability from osteoarthritis, people may avoid being physically active because of their pain and stiffness, confusion about how much and what to do, and not knowing when they will see benefits. Your physical therapist will be able to guide you in learning a personal exercise program that will help reduce your pain and stiffness.
Your physical therapist will work with you to:
- Reduce your pain
- Improve your leg, hip, and back motion
- Improve your strength, standing balance, and walking ability
- Speed healing and your return to activity and sport
Reduce Pain
Your physical therapist can use different types of treatments and technologies to control and reduce your pain, including ice, heat, ultrasound, electrical stimulation, taping, exercises, and hands-on (manual) therapy techniques, such as massage.
Improve Motion
Your physical therapist will choose specific activities and treatments to help restore normal movement in the leg and hip. These might begin with "passive" motions that the therapist performs for you to gently move your leg and hip joint, and progress to active exercises and stretches that you perform yourself. The physical therapist may use sustained stretches and manual therapy techniques that gently move the joint and stretch the muscles around the joint.
Improve Strength
Certain exercises will benefit healing at each stage of recovery; your physical therapist will choose and teach you the appropriate exercises to steadily restore your strength and agility. These may include using cuff weights, stretchy resistance bands, weight-lifting equipment, and cardio exercise equipment such as treadmills or stationary bicycles.
Speed Recovery Time
Your physical therapist will design a specific treatment program to speed your recovery. He or she is trained and experienced in choosing the right treatments and exercises to help you heal, return to your normal lifestyle, and reach your goals faster than you are likely to do on your own.
Return to Activities
Your physical therapist will design your treatment program to help you return to work or sport in the safest, fastest, and most effective way possible. You may engage in work re-training activities, or learn sport-specific techniques and drills to help you achieve your goals.
If Surgery Is Necessary
In severe cases of hip osteoarthritis, the hip joint degenerates until bone is rubbing on bone. This condition can require hip joint replacement surgery. Physical therapy is an essential part of postsurgical recovery, which can take several months.
If you undergo hip joint replacement surgery, your physical therapist will visit you in your hospital room to help you get out of bed and walk, and will explain any movements that you must avoid to protect the healing hip area.
He or she will work with you daily in the hospital and then in the clinic once you are discharged. He or she will be an integral part of your treatment and recoveries – helping you minimize pain, restore motion and strength, and return to normal activities in the speediest yet safest manner possible after surgery.
Can this Injury or Condition be Prevented?
Hip osteoarthritis may be prevented or limited by keeping the hip and leg muscles strong and flexible, maintaining a healthy body weight, and using proper balance skills. Research shows that strengthening and stretching exercises for the hip, core and leg can minimize and reduce osteoarthritis pain and stiffness, so it is reasonable to conclude that keeping those muscles strong and limber will help prevent painful osteoarthritis symptoms and problems.
When you seek help once hip osteoarthritis develops, your physical therapist can recommend a home exercise program to strengthen and stretch the muscles around your hip, upper leg, and abdomen to help prevent future hip pain and problems. These may include strength and flexibility exercises.
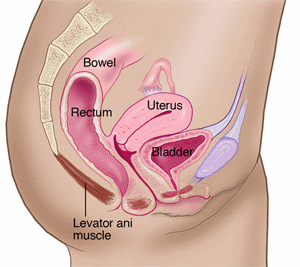
Pelvic pain is pain felt in the lower abdomen, pelvis, or perineum. It has many possible causes and affects up to 20% of the population in the United States, including women and men. Pelvic pain is considered "chronic" when it lasts for more than 6 months. Physical therapists help people experiencing pelvic pain restore strength and flexibility to the muscles and joints in the pelvic region, and reduce their pain.
What Is Pelvic Pain?
Pelvic pain can be caused by:
- Pregnancy and childbirth, which affect pelvic muscles and cause changes to pelvic joints
- Pelvic joint problems from causes other than pregnancy and childbirth
- Muscle weakness or imbalance within the muscles of the pelvic floor, trunk, or pelvis
- Changes in the muscles that control the bowel and bladder
- Tender points in the muscles around the pelvis, abdomen, low back, or groin areas
- Pressure on 1 or more nerves in the pelvis
- Weakness in the muscles of the pelvis and pelvic floor
- Scar tissue after abdominal or pelvic surgery
- Disease
- A shift in the position of the pelvic organs, sometimes known as prolapse
How Does it Feel?
The pain in your lower abdomen and pelvis may vary; some people say it feels like an aching pain; others describe it as a burning, sharp, or stabbing pain, or even pins and needles. In addition, you may have:
- Pain in the hip or buttock.
- Pain in the tailbone or pubic bone.
- Pain in the joints of the pelvis.
- Tender points in the muscles of the abdomen, low back, or buttock region.
- A sensation of heaviness in the pelvic region or even a sensation as if you are sitting on something hard, like a golf ball.
Signs and Symptoms
- Inability to sit for normal periods of time.
- Reduced ability to move your hips or low back.
- Difficulty walking, sleeping, or performing daily activities.
- Pain or numbness in the pelvic region with exercise or recreational activities, such as riding a bike or running.
- Pain during sexual activity.
- Urinary frequency, urgency, or incontinence, or pain during urination.
- Constipation or straining with bowel movements, or pain during bowel movements.
- Difficulty using tampons.
- Imbalance when walking.
How Is It Diagnosed?
Your physical therapist will complete a thorough review of your medical history, and perform a physical examination to identify the causes of your pelvic pain and any joint issues, muscle tightness or weakness, or nerve involvement. The exam may include:
- Pelvic girdle screening.
- Soft tissue assessment.
- Visual inspection of the tissues.
- Reflex testing.
- Sensation testing.
- Internal assessment of pelvic floor muscles.
Your physical therapist also will determine whether you should be referred to a physician to assist in your interdisciplinary plan of care.
How Can a Physical Therapist Help?
- Based on the examination results, your physical therapist will design an individualized treatment program to meet your specific needs and goals. Your physical therapist may:
- Show you how to identify the appropriate muscles, such as the pelvic floor, deep abdominals, and diaphragm.
- Educate you on how to use these muscles correctly for activities like exercise, posture correction, getting up from a chair, or squatting to pick up a child or pick something up from the floor.
- Teach you exercises to stretch and strengthen the affected muscles and retrain them, so they work together normally.
- Teach you techniques to improve blood flow and tissue function in the pelvic area.
- Teach you appropriate pelvic floor muscle exercises.
Depending on your symptoms and level of discomfort, your physical therapist may decide to use biofeedback to help make you aware of how your pelvic floor muscles work, and how you can control them better. Your physical therapist may attach electrodes to the area to measure your muscle activity as it displays on a monitor, and will work with you to help you understand and change those readings. Your physical therapist also may use gentle electrical stimulation to improve your awareness of your muscles.
Can this Injury or Condition be Prevented?
Some risk factors, such as aging, smoking and associated coughing, inactivity, obesity, or childbirth, affect general health and may affect core trunk and pelvic strength. Exercises, such as core stabilization, pelvic floor, and deep abdominal wall exercises, muscle flexibility training, and body awareness may help improve muscle function and lower the risk of pelvic injury or pain. See other resources to help you maintain health, such as Fitness Across the Lifespan, Fit After Fifty, Five Ways to Prepare Your Body for Pregnancy, and Nine Physical Therapist Tips to Help You Age Well.
Snapping hip syndrome refers to a snapping or popping sensation that occurs in the side, front, or back of your hip when you forcefully lift, lower, or swing your leg. Snapping hip makes it more difficult to perform activities such as lifting, kicking, or twisting your leg, getting up from a chair, walking, running or cycling. While the condition most often affects dancers and athletes, a snapping hip can occur in anyone performing forceful leg movements. Snapping hip is mostly seen in people 15 to 40 years of age.
What is Snapping Hip Syndrome?
Snapping hip occurs when a muscle, tendon, or ligament rolls over a bony prominence in the hip. Snapping hip can occur in different areas of the hip:
- Front. Snapping at the front of the hip can involve the hip flexor muscle rolling over the front of the hip bone, or the hip ligaments rolling over the thigh bone or tissues of the hip joint.
- Side. This condition involves the ITB (iliotibial band) rolling over the outer thigh bone or the big muscle on the back of the hip (gluteus maximus) sliding over the outer thigh bone.
- Back. This condition involves one of the hamstring muscles rolling over the bottom of the hip bone.
Snapping hip can occur when the hip muscles are excessively used and become fatigued, tight, and/or swollen.
Athletic activities like track and field, soccer, horseback riding, cycling, gymnastics, and dance can trigger the condition. It can also occur during everyday activities that require repeated forceful movement of the legs.
How Does it Feel?
Snapping hip causes a snapping sensation and sound that can be felt in the front, the side, or the back of the hip. Often, the snapping can be pain-free. If it causes pain, the pain usually ceases when the leg movement causing the snapping is stopped. In athletes and dancers, the snapping can be accompanied by weakness and may diminish performance.
The snapping is most commonly felt when kicking the leg forward or to the side, when bringing the leg behind the body, when rising from a chair, or when rotating the body or the leg.
Often, walking and running in a straight line are snap-free and pain-free, although in some people these activities are limited by the pain of the structure that is snapping.
Signs and Symptoms
With snapping hip, you may have:
- Snapping or popping in the front, side, or back of hip when lifting, lowering, or swinging the leg
- Weakness in the leg when trying to lift it forward or sideways
- Tightness in the front or back of the hip
- Swelling in the front or side of the hip
- Difficulty performing daily activities such as rising from a chair and walking
How Is It Diagnosed?
If you see your physical therapist first, the therapist will conduct a thorough evaluation that includes taking your health history. Your therapist will ask you:
- How you injured your hip and if you heard a pop when you suffered the injury
- If you feel snapping, popping, or pain
- Where you feel the snapping or pain
- If you experienced a direct hit to the leg
- If you saw swelling in the first 2 to 3 hours following the injury
- If you experience pain when lifting your leg forward or backward, walking, changing directions while walking or running, or when lifting the knee
- If you participate in any repetitive, forceful, or plyometric (quick explosive jumping) sport activities.
Your physical therapist also will perform special tests to help determine whether you have a snapping hip, such as:
- Asking you to lift your leg quickly
- Asking you to push against the physical therapist’s hand when he or she tries to push your leg outward, backward, and forward (muscle strength test)
- Gently feeling the muscle to determine the specific location of the injury (palpation)
Your therapist may use additional tests to assess possible damage to other parts of your body, such as your hip joint or lower back.
To provide a definitive diagnosis, your therapist may collaborate with a physician or other health care provider. The physician may order further tests—such as an x-ray or magnetic resonance imaging (MRI)—to confirm the diagnosis and also to rule out other potential damage. However, these tests are not commonly needed for snapping hip syndrome.
How Can a Physical Therapist Help?
Your physical therapist will design a specific treatment program to speed your recovery, including exercises and treatments you should perform at home. This program will help you return to your normal life and activities and reach your recovery goals.
The First 24-48 Hours
Your physical therapist may advise you to:
- Rest the injured hip by avoiding walking or any activity that causes pain. In rare cases, crutches may be recommended to reduce further strain on the muscles when walking.
- Apply ice packs to the affected area for 15 to 20 minutes every 2 hours.
- Consult with another health care provider for further services such as medication or diagnostic tests.
Reduce Pain
Your physical therapist can use different types of treatments and technologies to control and reduce your pain, including ice, heat, ultrasound, electricity, taping, exercises, and special hands-on techniques that move muscles and joints (manual therapy).
Improve Motion
Your physical therapist will choose specific activities and treatments to help restore normal movement in the leg and hip. These might start with movements of the leg and hip joint that the therapist gently performs, and progress to active exercises and stretches. Treatment for snapping hip often involves manual therapy techniques called trigger point release and soft tissue mobilization, as well as specific stretches to muscles that might be abnormally tight.
Improve Strength
Certain exercises will benefit your injury at each stage of recovery, and your physical therapist will choose and teach you the appropriate exercises that will restore your strength, power, and agility.
These may be performed using free weights, stretchy bands, weight-lifting equipment, and cardio exercise machines such as treadmills and stationary bicycles. For snapping hip syndrome, muscles of the hip and core are often targeted by the strength exercises.
Speed Recovery Time
Your physical therapist is trained and experienced in choosing the treatments and exercises to help you heal, get back to your normal life, and reach your goals faster than you might be able to on your own.
Return to Activities
Your physical therapist will collaborate with you to decide on your recovery goals, including return to work and sport, as well as design your plan of care to help you reach those goals in the safest, fastest, and most effective way possible. Your physical therapist will use hands-on therapy and teach you exercises and work retraining activities. Athletes will be taught sport-specific techniques and drills to help achieve sport-specific goals.
Prevent Future Re-injury
Your physical therapist can recommend a home exercise program to strengthen and stretch the muscles around your hip, upper leg, and core (abdomen) to help prevent future injury. These may include strength and flexibility exercises for the hip, thigh, and core muscles.
If Surgery Is Necessary
Surgery is rarely necessary in the case of snapping hip syndrome. If it is required, your physical therapist will help you minimize pain, restore motion and strength, and return to normal activities in the speediest manner possible after surgery.
Can this Injury or Condition be Prevented?
Snapping hip syndrome can be prevented by:
- Warming up before starting a sport or heavy physical activity. Your warm-up should include stretches taught to you by your physical therapist, including those for the muscles on the front, side, and back of the hip.
- Gradually increasing the intensity of an activity or sport. Avoid pushing too hard, too fast, too soon.
- Following a consistent strength and flexibility exercise program to maintain good physical conditioning, even in a sport’s off-season.
- Wearing shoes that are in good condition and fit well.
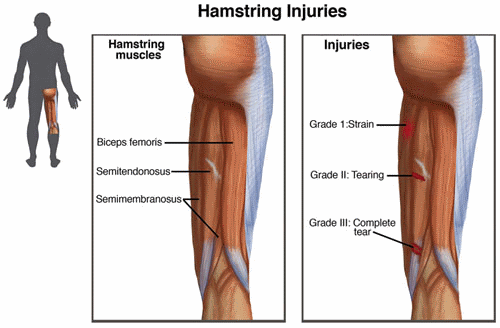
A hamstring injury occurs when 1 or more of the 3 hamstring muscles or tendons (a type of soft tissue connecting the muscle to the bone) tear. It is 1 of the most common injuries of the lower body, particularly affecting athletes participating in sports such as football, soccer, or track. After tearing a hamstring muscle, a person is 2 to 6 times more likely to suffer a subsequent injury. Surgery is required to treat the most severe cases. However, in most cases, hamstring injuries are managed with physical therapy.
What are Hamstring Injuries?
The hamstrings make up the primary muscle group responsible for straightening (extending) the hip and bending (flexing) the knee. It includes a group of 3 muscles along the back of the thigh that connect the pelvis to the leg. The three muscles are the:
- Semitendinosus
- Semimembranosus
- Biceps femoris
Hamstring injuries occur when excessive force is placed across the muscles. This typically happens during sudden starts or stops when running, a rapid change of direction with "cutting" or jumping maneuvers, or when the muscle is overstretched by activities such as sprinting, hurdling, kicking, or heavy lifting.
The common structures involved in hamstring injuries are:
- Hamstring muscle(s) and/or tendon (a type of soft tissue that connects muscle to bone)
- Bursa (a fluid-filled sack that sits between bones and soft tissues to limit friction), usually irritated with recurring hamstring injuries
- Ischial tuberosity (the "sit-bone"), which in rare cases can be fractured by traumatic injury
Risk factors for hamstring injuries include:
- A history of prior hamstring injury
- Muscle imbalances (particularly hamstring weakness)
- Poor flexibility (muscle tightness)
- Inadequate warm-up before activity
- Muscle fatigue
How Does it Feel?
When a person injures a hamstring muscle, the symptoms are related to the severity of the injury. Mild hamstring strains often just feel like a pulled or cramping muscle; you might not even realize you have pulled your hamstring until you stop performing the activity, or until the next day, when you might have soreness, tightness, or bruising. However, more involved injuries can be painful, and your symptoms might include:
- A sudden, sharp pain in the buttocks or back of the thigh
- A feeling of a "pop" or tearing in the muscle
- Bruising within hours or days after the injury
- Swelling
- Tenderness to touch
- Difficulty sitting comfortably, lifting the leg when lying down, or straightening the knee
- Difficulty walking, resulting in a limp
How Is It Diagnosed?
Diagnosis of hamstring injuries starts with a thorough understanding of your health history and the cause of the injury. The questions your therapist may ask include:
- If you have had a similar injury before
- What you were doing when you first felt the pain
- Where you felt the pain, and if you felt a "pop"
- If you noticed any swelling or bruising in the first 24 hours after the injury
- What you were able to do immediately following the injury, and how you have been functioning since the injury (walking, sleeping, lifting your leg, etc.)
Your physical therapist will also perform a clinical evaluation, including some of the following observations and tests to determine the nature of your injury:
- Observation: To note any discoloration or bruising
- Pain: To identify your current pain level, and the activities that make your pain better or worse
- Palpation: To pinpoint the location and size of the tender area through touch, which will help determine the severity of the injury
- Range of motion: To compare the motion of your injured leg with your healthy leg
- Muscle strength: To determine the strength of the hamstring muscles when bending or straightening your knee and hip
- Gait analysis: To note any limping or pain when walking
Typically, hamstring injuries are classified as Grade I – III depending on the severity of the injury.
- Grade I: Mild strain with minimal tearing; usually feels like a pulled or cramping muscle
- Grade II: Moderate strain with partial tearing; may cause a stinging or burning sensation at the back of the thigh
- Grade III: A severe, complete muscle tear; may result in a “lump” on the back of the thigh where the muscle has torn
If your physical therapist suspects a severe injury, you will likely be referred to an orthopedic physician for medical diagnostic imaging, including x-ray and MRI, to evaluate the extent of the injury. In the event of a fracture of the ischial tuberosity (sit-bone) and/or a complete rupture of the muscle, surgery might be recommended.
How Can a Physical Therapist Help?
Your physical therapist will design an individualized treatment program specific to the exact nature of your injury and your goals.
The First 24-48 hours
Physical therapy may include:
- Resting the injured area by avoiding aggravating activities, such as walking or working out. If you are having notable difficulty walking, crutches may be recommended.
- Applying ice to the injured area 3-4x/day for 15-20 minutes (with a towel placed between your skin and the ice).
- Applying a compression wrap to the area to aid in decreasing swelling and pain.
- Referral to another health care provider for further diagnostic testing (if needed).
Range of motion
It is common for muscles and joints to become stiff after an injury. As your pain decreases, your physical therapist will begin gentle flexibility exercises, such as stretching your hamstring muscles.
Muscle strength
Hamstring strengthening will be an essential part of your rehabilitation program. Your physical therapist will compare the strength of the muscle groups in each leg, and prescribe specific exercises to target areas of weakness.
Manual therapy
Many physical therapists are trained in hands-on "manual" therapy to move and manipulate muscles and joints to improve motion, flexibility, and strength. These techniques can target areas that are difficult to treat on your own.
Functional training
As you regain the flexibility and strength in your hamstrings, it will be important to teach your body how to move so you no longer put excessive stress on the previously injured area. Your physical therapist will develop a functional training program specific to your desired activity.
In the event that the severity of your hamstring injury requires surgical treatment, a physical therapist will guide your postoperative rehabilitation. Your physical therapist will communicate with your surgeon to ensure complete and consistent postoperative care.
Can this Injury or Condition be Prevented?
You can decrease your risk of a hamstring injury in the following ways:
- Always warm up before participating in athletic activities.
- Avoid starting a new activity too quickly; gradually increase the frequency and intensity of the activity so that your body may adapt to the new movement patterns.
- Listen to your body after you work out (and stretch, apply ice, rest as needed) prior to engaging in the same routine again.
- Use proper lifting and squatting techniques, particularly when maneuvering heavy objects.
