-
 Injury keeping you out of the game?Our experts will get to the core of your fitness needs.OUR SERVICES
Injury keeping you out of the game?Our experts will get to the core of your fitness needs.OUR SERVICES -
 GET BACK TO THE ACTIVITIES YOU LOVEOUR SERVICES
GET BACK TO THE ACTIVITIES YOU LOVEOUR SERVICES -
 RESTORING YOUR PHYSICAL ABILITYOUR SERVICES
RESTORING YOUR PHYSICAL ABILITYOUR SERVICES -
 RESTORING YOUR QUALITY OF LIFEOUR SERVICES
RESTORING YOUR QUALITY OF LIFEOUR SERVICES -
 EVIDENCE BASED PRACTICEOUR SERVICES
EVIDENCE BASED PRACTICEOUR SERVICES -
 APPROPRIATE PROGRAM FOR A SUCCESSFUL RECOVERYOUR SERVICES
APPROPRIATE PROGRAM FOR A SUCCESSFUL RECOVERYOUR SERVICES -
 HELPING YOU ACHIEVE YOUR GOALSOUR SERVICES
HELPING YOU ACHIEVE YOUR GOALSOUR SERVICES
Knee
An anterior cruciate ligament (ACL) tear is an injury to the knee commonly affecting soccer players, basketball players, skiers, gymnasts, and other athletes. About 70% of ACL tears are the result of non-contact injuries; 30% are the result of direct contact (player-to-player, player-to-object). Women are 4-6 times more likely than men to experience an ACL tear.
Usually, you will be examined by a physical therapist or an orthopedic surgeon immediately following injury. Most people who sustain an ACL tear will undergo surgery to repair the tear; however, some people may avoid surgery by modifying their physical activity so that they don't put a lot of stress on the knee. A select group can actually return to vigorous physical activity following rehabilitation without having surgery.
Your physical therapist, together with your surgeon, can help you determine if non-operative treatment (rehabilitation without surgery) is a reasonable option for you. If you elect to have surgery, your physical therapist will help you both prepare for surgery and recover your strength and movement following surgery.
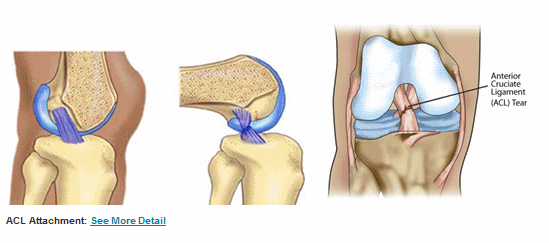
What is an ACL Tear?
The ACL is one of the major ligaments (bands of tissue) connecting the thigh bone to the shin bone. It can tear if you:
- Twist your knee while keeping your foot planted on the ground
- Stop suddenly while running
- Suddenly shift your weight from one leg to the other
- Jump and land on an extended (straightened) knee
- Stretch the knee farther than you should
- Experience a direct hit to the knee
How Does it Feel?
When you tear the ACL, you may feel a sharp, intense pain or hear a loud "pop" or snap. You might not be able to walk on the injured leg because you can’t support your weight through your knee joint. Usually, the knee will swell immediately (within minutes to a few hours), and you might feel that your knee "gives way" when you walk or put weight on it.
How Is It Diagnosed?
If you see your physical therapist first, your therapist will conduct a thorough evaluation that includes reviewing your health history. Your therapist will ask you whether you:
- Felt pain or heard a pop when you jumped, stopped quickly when running, turned your leg with your foot on the ground, or stretched your knee farther than usual
- Had a direct hit to the leg while your foot was planted on the ground
- Saw severe swelling around the knee in the first 2-3 hours following the injury
- Felt your knee buckling or giving way when you tried to get up from a chair, walk up and down stairs, or turn while walking
Your physical therapist also will perform special tests to help determine the likelihood that you have an ACL tear. For instance, the therapist may bend your knee and gently pull on the lower leg (called the "anterior drawer" test or the "Lachman" test). The therapist also might use the "pivot shift" test, gently bending and twisting your knee at the same time. (You might feel some discomfort or instability during these tests, which is normal.) Your therapist may use additional tests to assess possible damage to other parts of your knee.
The orthopedic surgeon may order further tests, including magnetic resonance imaging (MRI), to confirm the diagnosis and also to rule out other possible damage to the knee.
How Can a Physical Therapist Help?
Once an ACL tear has been diagnosed, you will work with your surgeon and physical therapist to decide if you should have surgery or if you can try to manage your recovery without surgery. If you don’t have surgery, your therapist will work with you to restore your muscle strength, endurance, and coordination so that you can return to your regular activities. In some cases, the therapist may help you to learn to modify your physical activity so that you put less stress on your knee. If you decide to have surgery, your therapist can help you both before and after the procedure.
Treatment Without Surgery
Current research evidence has identified a specific group of patients (called "copers") who have the potential for success without surgery. These patients have injury only to the ACL, and no episodes of "giving way" since the initial injury. There are specific functional tests—such as the Knee Outcomes Survey, the Global Rating of Knee Function, and the timed hop test—that can help the physical therapist identify this group of patients. If you fall into this category, your physical therapist will design a specific physical therapy treatment program for you, most likely including electrical stimulation to the quadriceps muscle, cardiovascular strengthening, traditional muscle strengthening, and balance training.
Treatment Before Surgery
Some orthopedic surgeons refer their patients to a physical therapist for a short course of rehabilitation before surgery. Your therapist will help you decrease your swelling, increase the range of movement of your knee, and strengthen your thigh muscles (quadriceps).
You might have what is known as a "quadriceps lag." This is when you try to raise your leg straight in the air, but you can't control the knee, and your leg bends slightly. Research shows that improving this condition before surgery leads to better outcomes after surgery. Your therapist might use electrical stimulation to help you straighten your leg.
Treatment After Surgery
Your orthopedic surgeon will provide postsurgery instructions. Physical therapists have developed and published guidelines on knee stability and movement problems, which recommend the following actions.
Bearing weight. Immediately after surgery, you will use crutches to walk. The amount of weight you are allowed to put on your leg and how long you use the crutches will depend on the type of reconstructive surgery you had. Your physical therapist will guide you through this part of your rehabilitation.
Icing and compression. Immediately after your surgery, your physical therapist will control your swelling with a cold application, such as an ice sleeve that fits around your knee and compresses it.
Bracing. Almost all surgeons will give you a brace to limit your knee movement (range of motion) after your surgery. Some will give you a brace to use during sports a little further along during your recovery. Your physical therapist will fit you with the brace and teach you how to use it safely.
Exercises to increase your ability to move. You will begin some exercises almost immediately following surgery. In the first week, your physical therapist will help you with your range of motion and teach you gentle exercises that you can do at home. The focus will be on regaining full movement of your knee. If you're like most people, this will take some time.
You will do exercises without pressure on your leg (called "non-weight-bearing exercises") and ones that have you placing weight on your leg ("weight-bearing exercises"). These exercises might be limited to a specific range of motion to protect your newly healing ACL graft. Your therapist might use electrical stimulation to help restore your quadriceps (thigh) muscle strength and help you achieve those last few degrees of straightening the knee.
Exercises to increase your strength. In the first 4 weeks after surgery, your physical therapist will help you increase your ability to put weight on your knee, using a combination of weight-bearing and non-weight-bearing exercises. The exercises will focus on your quadriceps and hamstrings (thigh muscles) and might be limited to a specific range of motion to protect the new ACL. Your therapist might use electrical stimulation to help restore your quadriceps strength.
During weeks 5 through 12, you can expect to begin to walk without crutches and regain a normal walking pattern. Your therapist will increase the intensity of your exercises and add balance exercises to your program. After 3-4 months, your thigh muscles should have about 75% of the strength of the muscles on your uninjured side. During this time, you and your therapist will be planning your return to higher-level activity.
Return to your sport or physical activity. You may begin balance exercises, running, jumping, hopping, and other exercises specific to your sport. This phase varies greatly from person to person. One study found that the return to moderate and strenuous sports varied between 6 and 12 months after surgery. You might be ready to return to your sport if:
- You no longer have pain and swelling
- You have no feelings of instability during sport-specific activities, such as cutting, jumping, and landing
- Your quadriceps strength is 90% of that on your uninjured side
- Your performance of the 1-legged hop test is at 90% of that on the uninjured side
Remember, each surgeon might have a specific plan for you; these are only broad guidelines describing what you might expect for your recovery.
Can this Injury or Condition be Prevented?
Current research shows that the percentage of ACL tears has been reduced in certain populations. Much of the research on ACL tears has been conducted with female collegiate athletes, because women are 4-6 times more likely to have this injury. Preventative physical therapy programs have proven to lower ACL injury rates by 41% for female soccer players. Researchers have made the following recommendations for a preventive exercise program:
- The program should be designed to improve balance, strength, and sports performance. Strengthening your core (abdominal) muscles is key to preventing injury, in addition to strengthening your thigh and leg muscles.
- Exercises should be done 2 or 3 times per week and should include sport-specific exercises.
- The program should last no fewer than 6 weeks.
Although most exercise studies have been conducted with female athletes, the findings may benefit male athletes as well.
Knee bursitis, commonly known as "housemaid's knee" and "clergyman's knee," involves swelling of 1 or more of the bursae at the front of the knee. Knee bursitis is one of the most common bursitis conditions; it can be painful when moving the knee, when kneeling, or even when at rest. The condition can also be painless, with only visible swelling present. Knee bursitis can have many causes. The most common is trauma, whether from a direct hit, or the result of activities that require crawling or kneeling on hard surfaces for long periods of time, such as laying carpet or tile, or scrubbing floors. Knee bursitis is most commonly seen in athletes; up to 10% of runners develop knee bursitis. However, its occurrence is not related to any particular age or ethnic group, and can also be caused by infection or autoimmune conditions. Physical therapists treat individuals with knee bursitis to reduce their pain, swelling, stiffness, and any associated weakness in the knee or leg.
What is Knee Bursitis?
Knee bursitis (also called prepatellar or infrapatellar bursitis) occurs when 1 or more of the many bursae (fluid-filled sacs) becomes damaged, irritated, or inflamed. Normally, a bursa acts as a cushion or friction-reducer between 2 body parts, such as between bone and skin, or bone and ligament or tendon. Bursae on the front of the knee serve as cushions between the knee cap and skin, and between the patellar tendon and tibia bone. Prolonged pressure or traumatic blows can injure a bursa, and repetitive motions can cause irritating friction on it, leading to the development of bursitis. In fact, "itis" means "inflammation." When the bursa is injured, it can swell and become painful.
Knee bursitis can be caused by:
- Repetitive motions, including certain sports, such as running
- Prolonged kneeling, as when cleaning floors, installing flooring, or praying in a kneeling position
- Prolonged crawling, such as when laying carpet or flooring, or scrubbing floors
- Direct trauma, such as being hit or falling on the knee
- Knee surgery or knee joint replacement
- Infection
- Autoimmune conditions
With knee bursitis, you may experience:
- Swelling on the front of the knee
- Redness on the front of the knee
- Pain when you push with your fingers on the front of the knee
- Pain when kneeling
- Stiffness in the knee joint, or difficulty straightening or bending the knee
How Is It Diagnosed?
If you see your physical therapist first, your therapist will conduct a thorough evaluation that includes taking your health history. Your physical therapist also will ask you detailed questions about your injury, such as:
- How and when did you notice the swelling and/or pain?
- Have you been performing any repetitive activity?
- Did you receive a direct hit to the knee, fall on it, or kneel for a long period of time?
Your physical therapist also will perform special tests to help determine the likelihood that you have knee bursitis. Your physical therapist will gently press on the front of the knee to see if it is painful to the touch, and may use additional tests to determine if other parts of your knee are injured. Your therapist also will observe how you can move your knee, and test your strength and flexibility.
Your physical therapist will test and screen for other, more serious conditions that could cause knee pain or swelling. To provide a definitive diagnosis, your physical therapist may collaborate with an orthopedic physician or other health care provider, who may order further tests to confirm the diagnosis and to rule out other damage to the knee, such as a fracture or infection.
How Can a Physical Therapist Help?
Your physical therapist will work with you to design a specific treatment program that will speed your recovery, including exercises and treatments that you can do at home. Physical therapy will help you return to your normal lifestyle and activities. The time it takes to heal the condition varies, but results can be achieved in 2 to 8 weeks or less, when a proper swelling management, stretching, and strengthening program is implemented.
During the first 24 to 48 hours following your diagnosis, your physical therapist may advise you to:
- Apply light compression to the area by wrapping the knee a specific way using a compressive wrap.
- Rest the area by avoiding any activity that causes pressure or pain in the knee.
- Apply ice packs to the area for 15 to 20 minutes every 2 hours.
- Consult with a physician for further services, such as medication or diagnostic tests.
Your physical therapist will work with you to:
Reduce Pain and Swelling. If repetitive activities have caused the knee bursitis, your physical therapist will help you understand how to avoid or modify the activities to allow healing to begin. Your physical therapist may use different types of treatments and electrothermal modalities (machines that use heat, light, or sound to reduce swelling and pain) to control and reduce your pain and swelling.
Improve Motion. Your physical therapist will choose specific activities and treatments to help restore normal movement in the knee and leg. These might begin with "passive" motions that the therapist performs for you to gently move your knee joint, and progress to active exercises and stretches that you do yourself.
Improve Flexibility. Your physical therapist will determine if any of your leg muscles are tight, start helping you to stretch them, and teaching you how to stretch them on your own.
Improve Strength. If your physical therapist finds any weak or injured leg muscles, your therapist will choose and teach you the correct exercises and equipment to steadily restore your strength and agility.
Improve Endurance. Restoring your leg's muscular endurance is important after an injury. Your physical therapist will develop a program of activities to help you regain the endurance that you had before the injury, so you can return to doing the things you like to do.
Improve Balance. Regaining your sense of balance is important after an injury. Your physical therapist will teach you exercises to improve your balance skills.
Restore Agility. Speed and accuracy of leg movement is important in athletics. Your physical therapist will help you regain these skills in preparation for a return to sports activities.
Learn a Home Program. Your physical therapist will teach you strengthening and stretching exercises to perform at home. These exercises will be specific for your needs; if you do them as prescribed by your physical therapist, you can speed your recovery.
Return to Activities. Your physical therapist will discuss your activity goals with you and use them to set your work, sport, and home-life recovery goals. Your treatment program will help you reach your goals in the safest, fastest, and most effective way possible. Your physical therapist will teach you exercises, work retraining activities, and sport-specific techniques and drills to help you achieve your goals.
Speed Recovery Time. Your physical therapist is trained and experienced in choosing the best treatments and exercises to help you safely heal, return to your normal lifestyle, and reach your goals faster than you are likely to do on your own.
If Surgery Is Necessary
Surgery is not commonly required for knee bursitis. But if surgery is needed, you will follow a recovery program over several weeks, guided by your physical therapist. Your physical therapist will help you minimize swelling and pain, regain motion and strength, and return to normal activities in the safest and speediest manner possible.
Knee pain can be caused by disease or injury. The most common disease affecting the knee is osteoarthritis. Knee injuries can occur as the result of a direct blow or sudden movement that strains the knee beyond its normal range of movement. Knee pain caused by an injury is most often associated with knee cartilage tears, such as meniscal tears, or ligament tears, such as anterior cruciate ligament tears.
What is Knee Pain?
Knee pain can be caused by disease or injury. Knee pain can restrict movement, affect muscle control in the sore leg, and reduce the strength and endurance of the muscles that support the knee.
The most common disease affecting the knee is osteoarthritis, which is caused by the cartilage in the knee gradually wearing away, resulting in pain and swelling.
Knee injuries can occur as the result of a direct blow or sudden movement that strains the knee beyond its normal range of motion, as can happen in sports, recreational activities, a fall, or a motor vehicle accident. Knee pain caused by an injury often is associated with tears in the knee cartilage or ligaments. Knee pain also can be the result of repeated stress, as often occurs with the kneecap, also known as patellofemoral pain syndrome. Very rarely, with extreme trauma, a bone may break at the knee.
You may feel knee pain in different parts of your knee joint, depending on the problem affecting you. Identifying the location of your pain can help your physical therapist determine its cause.
How Is It Diagnosed?
Your physical therapist will make a diagnosis based on your symptoms, medical history, and a thorough examination. X-ray and magnetic resonance imaging (MRI) results may also be used to complete the diagnosis.
To help diagnose your condition, your physical therapist may ask you questions like these:
- Where exactly on your knee is the pain?
- Did you twist your knee?
- Did you feel a "tearing" sensation at the time of injury?
- Do you notice swelling?
- Have you ever felt like your knee joint is "catching," or "locking," or will give way?
- Do you have difficulty walking up and down stairs?
- Do you have difficulty sitting with your knee bent for long periods, as on an airplane or at the movies?
- Does your pain increase when you straighten or bend your knee?
- Does your knee hurt if you have to twist or turn quickly?
The physical therapist will perform tests to find out whether you have:
- Pain or discomfort with bending or straightening your knee
- Tenderness at the knee joint
- Limited motion in your knee
- Weakness in the muscles around your knee
- Difficulty putting weight on your knee when standing or walking
The physical therapist also is concerned about how well you are able to use your injured knee in daily life. To assess this, the therapist may use such tests as a single-limb hop test, a 6-minute walk test, or a timed up and go test.
How Can a Physical Therapist Help?
Based on the evaluation, your physical therapist will develop a customized rehabilitation program, including a specific set of knee exercises, for you.
If you already have knee problems, your physical therapist can help with a plan of exercise that will strengthen your knee without increasing the risk of injury or further damage. As a general rule, you should choose gentle exercises such as swimming, aquatic exercise, or walking rather than jarring exercises such as jogging or high-impact aerobics.
Consult your physical therapist about specific ways to maintain your knee health following injury or surgery. Your physical therapist has the relevant educational background and expertise to evaluate your knee health and to refer you to another health care provider if necessary.
Depending on the severity of your knee problem, your age, and your lifestyle, the therapist may select such treatments as:
Strength training and functional exercises, which are designed to increase strength, endurance, and function of your leg muscles (quadriceps and hamstrings). This in turn helps support the knee and reduce stress to the knee joint.
Electrical stimulation of the knee, which further increases leg muscle strength and can help reduce knee pain. To increase strength, electrical impulses are generated by a device and delivered through electrodes to stimulate the primary muscle that supports the knee, the quadriceps femoris. To reduce your knee pain, the electrodes are placed on the skin to gently stimulate the nerves around the knee.
Your physical therapist can determine just how much you may need to limit physical activity involving the affected knee. He or she also can gauge your knee’s progress in function during your rehabilitation.
How Can a Physical Therapist Help Before & After Surgery?
Your physical therapist, in consultation with your surgeon, will be able to tell you how much activity you can do depending on the type of knee surgery (such as total knee replacement) you undergo. Your therapist and surgeon also might have you participate in physical therapy prior to surgery to increase your strength and motion. This can sometimes help with recovery after surgery.
Following surgery, your physical therapist will design a personalized rehabilitation program for you and help you gain the strength, movement, and endurance you need to return to performing the daily activities you did before.
Lateral collateral ligament (LCL) sprain occurs when the ligament on the outer side of the knee is overstretched. Collateral ligament knee injuries make up about 25% of severe knee injuries in the United States. They most often occur in adults aged 20-34 years and 55-65 years. LCL sprains mainly happen during sporting activities, including contact and noncontact sports, and affect women and men equally. A physical therapist treats LCL sprains to reduce pain, swelling, stiffness, and any associated weakness in the knee or lower extremity.
The LCL can be injured if the knee is hit on the inner side, which pushes the knee outward, or if the knee straightens too quickly or forcefully (hyperextends), which causes stress on the outer side of the knee. The LCL may be stretched, partially torn, or completely torn.
How Does it Feel?
With an injured LCL, you may feel:
- Swelling on the outside of the knee
- Pain on the outside of the knee
- Tenderness on the outside of the knee
- A feeling that the knee is locking, catching, buckling or giving way during movement
The pain of an LCL injury may cause you to limp.
How Is It Diagnosed?
If you see your physical therapist first, your therapist will conduct a thorough evaluation that includes taking your health history. Your physical therapist will also ask you detailed questions about your injury, such as:
- How and when did you notice the pain?
- Did you feel pain or hear a "pop" when you injured your leg?
- Did you turn your leg with your foot planted on the ground?
- Did you change direction quickly while running?
- Did your knee straighten out very quickly?
- Did you receive a direct hit to the leg while your foot was planted on the ground?
- Did you see swelling around the knee in the first 2 to 3 hours following the injury?
- Does your knee feel like it is locking, catching, buckling, or giving way when you try to use it?
Your physical therapist also will perform special tests to help determine the likelihood that you have an LCL sprain. Your physical therapist will gently press on the outer side of your knee to see if it is painful to the touch, and push on the inner side of the knee to see if that causes pain on the outer side. Your physical therapist may use additional tests to determine if other parts of your knee are injured, and will also observe how you are walking.
To provide a definitive diagnosis, your physical therapist may collaborate with an orthopedic physician or other health care provider. They may order further tests, such as an x-ray to confirm the diagnosis and to rule out other damage to the knee, including fracture.
How Can a Physical Therapist Help?
Your physical therapist will work with you to design a specific treatment program that will speed your recovery, including exercises you can do at home. Physical therapy will help you return to your normal lifestyle and activities. The time it takes to heal the condition varies, but improvement is generally noted in 4 to 6 weeks.
During the first 24 to 48 hours following your injury, your physical therapist may advise you to:
- Rest the area by using crutches or a brace, or by avoiding walking or any activity that causes pain.
- Apply ice packs to the area for 15–20 minutes every 2 hours.
- Consult with a physician for further services, such as medication or diagnostic tests.
Your physical therapist will work with you over time to:
Reduce Pain and Swelling
Your physical therapist may use different types of treatments and technologies to control and reduce your pain and swelling, including ice, heat, ultrasound, electrical stimulation, taping, exercises, and hands-on therapy, such as massage.
Improve Motion
Your physical therapist will choose specific activities and treatments to help restore normal movement in the knee and leg. These might begin with "passive" motions that your physical therapist performs for you to gently move your leg and knee joint, and progress to active exercises and stretches that you do yourself.
Improve Flexibility
Your physical therapist will determine if any of your leg muscles are tight, and teach you how to stretch them.
Improve Strength
Certain exercises will aid healing at each stage of recovery. Your physical therapist will choose the exercises and equipment that are right for your specific condition to steadily restore your strength and agility. These may include cuff weights, stretch bands, weight-lifting equipment, and cardio-exercise equipment, such as treadmills or stationary bicycles.
Improve Balance and Agility
Regaining your sense of balance is important after an injury. For athletes, restoring agility is important, also. Your physical therapist will teach you exercises to improve your balance and agility skills.
Speed Recovery Time
Your physical therapist is trained and experienced in choosing the best treatments and exercises to help you heal, return to your normal lifestyle, and reach your goals faster than you are likely to do on your own.
Return to Activities
Your physical therapist will discuss your goals with you and use them to set your work, sport, and home-life recovery goals. Your treatment program will help you reach those goals in the safest, fastest, and most effective way possible. Your physical therapist will teach you exercises, work retraining activities, and sport-specific techniques and drills to help you achieve your goals.
If Surgery Is Necessary
Surgery is extremely rare in cases of LCL injury. However, if other parts of the knee are injured at the same time as the LCL, you may need additional treatment for those injuries that might include surgery. If surgery is needed, you will follow a recovery program over several weeks guided by your physical therapist, who will help you minimize pain, regain motion, strength and agility, and return to normal activities in the speediest manner possible.
Can this Injury or Condition be Prevented?
Your physical therapist can recommend a home exercise program to strengthen and stretch the muscles around your knee, upper leg, and abdomen to help prevent future injury. These may include strength and flexibility exercises for the leg, knee, and core (midsection) muscles.
To help prevent a recurrence of the injury, your physical therapist may advise you to:
- Learn correct knee positioning when participating in athletic activities.
- Follow a consistent flexibility and strength exercise program, especially for the hamstrings (back of the thigh) and quadriceps (front of the thigh) muscles, to maintain good physical conditioning, even in a sport's off-season.
- Practice balance and agility exercises and drills.
- Always warm up before starting a sport or heavy physical activity.
- Wear shoes that are in good condition and fit well.
- Maintain a healthy weight.
The medial collateral ligament (MCL) is the most commonly damaged ligament in the knee. The MCL can be sprained or torn as a result of a blow to the outer side of the knee, by twisting the knee, or by quickly changing directions while walking or running. MCL injury most often occurs in athletes, although nonathletes can also be affected. A physical therapist treats an MCL sprain or tear to reduce pain, swelling, stiffness, and any associated weakness in the knee or lower extremity.
What is an MCL Injury?
The MCL is a small, thick band of tissue on the inner side of the knee joint. It connects two bones—the thighbone and the shin bone—preventing the knee from bending inward toward the other knee. When the knee is hit on the outer side of the leg (eg, the left side of the left leg), or if the knee is twisted violently, the MCL can overstretch resulting in a partial or complete tear. MCL injuries commonly occur in football players who get "clipped" or hit on the outer side of the knee. Other causes may include twisting and turning while skiing, blows received on the soccer field, trauma experienced in a car accident, or simply turning the knee sharply while the foot is planted on the ground. Healing times vary from a couple of weeks to a couple of months, depending on the severity of the injury.
How Does it Feel?
When you experience an MCL injury, you may feel:
- Pain on the inner side of the knee
- Swelling and bruising at the inner side of the knee
- Swelling that spreads to the rest of the knee joint in 1 or 2 days following injury
- Stiffness in the knee
- Difficulty or pain when trying to bend or straighten the knee
- An unstable feeling, as though the knee may give out or buckle
- Pain or difficulty walking, sitting down, rising from a chair, or climbing stairs
Signs and Symptoms
With an MCL injury, you may experience
- A "popping" sound as the injury occurs
- Pain and swelling in your knee
- Difficulty moving your knee
- Difficulty bearing weight on your leg for walking or getting up from a chair
How Is It Diagnosed?
If you see your physical therapist first, the therapist will conduct a thorough evaluation that includes taking your health history. Your therapist will also ask you detailed questions about your injury, such as:
- Did you feel pain or hear a "pop" when you injured your leg?
- Did you turn your leg with your foot planted on the ground?
- Did you change direction quickly while running?
- Did you receive a direct hit to the leg while your foot was planted on the ground?
- Did you see swelling around the knee in the first 2 to 3 hours following the injury?
- Does your knee feel like buckling or giving way when you try to use it?
Your physical therapist also will perform special tests to help determine the likelihood that you have an MCL injury. Your therapist will gently press on the outside of your knee while it is slightly bent as well as when it is fully straight to test the strength of the ligament. The therapist will also check the inner side of your knee for tenderness and swelling and measure for swelling with a tape measure. The therapist may use additional tests to determine if other parts of your knee are injured, and will also observe how you are walking.
To provide a definitive diagnosis, your therapist may collaborate with an orthopedic physician or other health care provider. The orthopedic physician may order further tests, such as magnetic resonance imaging (MRI), to confirm the diagnosis and to rule out other damage to the knee. It also helps to determine whether surgery is required. MRI is not required in all cases but may be ordered. Your therapist or doctor may recommend a knee brace, a knee immobilizer, or crutches to reduce pain if the MCL injury is severe
How Can a Physical Therapist Help?
Your physical therapist will work with you to design a specific treatment program that will speed your recovery, including exercises and treatments you can do at home. Physical therapy will help you return to your normal lifestyle and activities.
The First 24-48 Hours
Your physical therapist may advise you to:
- Rest the area by avoiding walking or any activity that causes pain. Crutches and a knee brace may be recommended to reduce further strain on the MCL when walking.
- Apply ice packs to the area for 15-20 minutes every 2 hours.
- Compress the area with an elastic bandage wrap.
- Consult with a physician for further services such as medication or diagnostic tests.
Reduce Pain
Your physical therapist may use different types of treatments and technologies to control and reduce your pain, including ice, heat, ultrasound, electrical stimulation, taping, exercises, and hands-on therapy such as massage.
Improve Motion
Your physical therapist will choose specific activities and treatments to help restore normal movement in the knee and leg. These might begin with passive motions that the therapist performs for you to gently move your leg and knee joint, and progress to active exercises and stretches that you do yourself.
Improve Strength
Certain exercises will aid healing at each stage of recovery; your physical therapist will choose and teach you the correct exercises and equipment to steadily restore your strength and agility. These may include using cuff weights, stretchy bands, weight-lifting equipment, and cardio-exercise equipment such as treadmills or stationary bicycles.
Improve Balance
Regaining your sense of balance is important after an injury. Your physical therapist will teach you exercises to improve your balance skills.
Speed Recovery Time
Normal healing of time is a few weeks to a few months, depending on which tissues are injured and how severely they are injured. Your physical therapist is trained and experienced in choosing the right treatments and exercises to help you heal, return to your normal lifestyle, and reach your goals faster than you are likely to do on your own.
Return to Activities
Your physical therapist will discuss your goals with you and use them to set your work, sport, and homelife recovery goals. The therapist will design your treatment program to help you reach those goals in the safest, fastest, and most effective way possible. Your physical therapist will apply hands-on therapy, such as massage, and teach you exercises, work retraining activities, and sport-specific techniques and drills to help you achieve your goals.
Prevent Future Injury
Your physical therapist can recommend a home exercise program to strengthen and stretch the muscles around your knee, upper leg, and abdomen to help prevent future injury. These may include strength and flexibility exercises for the leg, knee, and core muscles.
If Surgery Is Necessary
Surgery is rarely necessary in the case of an MCL injury. If surgery is needed, you will follow a recovery program over several weeks guided by your physical therapist, who will help you minimize pain, regain motion, strength, and return to normal activities as quickly as possible after surgery.
Can this Injury or Condition be Prevented?
To help prevent a recurrence of the injury, your physical therapist may advise you to:
- Learn how to not let your knees collapse in toward each other when jumping, running, or turning quickly
- Practice balance and agility exercises and drills
- Always warm up before starting a sport or heavy physical activity
- Follow a consistent strength and flexibility exercise program to maintain good physical conditioning, even in a sport's off-season
- Wear shoes that are in good condition and fit well
The medial patellofemoral ligament (MPFL) helps to keep the kneecap centered along the front of the knee, so that it tracks well during knee movements. MPFL injuries typically occur during a forceful traumatic kneecap dislocation. This injury is most common among young, active females. Depending on the severity of an MPFL injury, treatment may involve surgical reconstruction, followed by physical therapy. Physical therapists design treatment programs for individuals with MPFL injuries to help them gently restore their knee strength and function.
What is a Medial Patellofemoral Injury?
The medial patellofemoral ligament is a broad structure located on the inside of the knee joint. It connects the kneecap (patella) to the thigh bone (femur). The primary purpose of the MPFL is to provide stability to the kneecap; it provides restraint to any movement toward the outside of the knee. It also helps keep the kneecap in position, as the knee bends and straightens.
How Does it Feel?
Common signs and symptoms that may occur with an MPFL injury include:
- Feeling the knee “giving way” or “buckling” during activity.
- Feeling like the kneecap is sliding out to the side during knee movement.
- Swelling of the knee following activity.
- Restricted joint movement (range of motion).
- Pain when moving the joint.
- Tenderness to touch along the affected joint.
- Pain, stiffness, or "locking," after sitting with the knee bent or straight for a prolonged period of time.
How Is It Diagnosed?
When you first go to see your physician or physical therapist, the therapist will review your medical history, ask you how and when you injured your knee, and ask you to describe your symptoms. Your physical therapist will perform a comprehensive physical exam of your knee, assessing different measures, such as range of motion, strength, and flexibility. The physical therapist likely will manipulate your knee, placing it in certain positions to try to pinpoint which specific structures may be injured. If an MPFL injury is suspected, your physical therapist may assess the mobility of your kneecap, specifically to note if it moves more to the outside compared to your uninjured knee. Additionally, you may be asked to briefly perform or describe the activities that cause your pain.
Imaging techniques, such as x-rays or an MRI, may be required to gain a more thorough and objective evaluation of all of the structures of the knee joint. Your physical therapist may refer you to an orthopedic physician for further investigation, if needed.
How Can a Physical Therapist Help?
Your physical therapist will design an individualized treatment program specific to the exact nature of your condition and your goals. Your treatment may include:
Range-of-Motion Exercises. Many individuals who develop MPFL laxity or injury are naturally flexible. However, when there is an injury to a joint, our bodies tend to become guarded, which may limit the joint’s range of motion. Your physical therapist will assess your motion compared to expected normal motion and the motion of the uninvolved joint on the other side of your body. Your physical therapist will prescribe range-of-motion exercises to help restore natural movement to the knee.
Muscle Strengthening. Strengthening the muscles around the injured joint is an essential part of the rehabilitation program. As the muscles along the front and back of the thigh (the quadriceps and hamstrings) cross the knee joint, they help control the motion and forces that are applied to the bones of the knee. When there is an injury to a joint that causes pain and swelling, muscles often become inhibited, which means they may not function at their normal capacity. Strengthening the hip and core muscles also can help balance the amount of force on the joints of the leg, particularly during walking or running. Your physical therapist will assess these different muscle groups, compare the strength in each limb, and prescribe specific exercises to target your areas of weakness.
Manual Therapy. Physical therapists are trained in manual (hands-on) therapy. Your physical therapist will gently move and manipulate your muscles and joints to improve their motion, flexibility, and strength. These techniques can target areas that are difficult to treat on your own. For patients with MPFL injuries, manual therapy techniques can help restore the joint's normal motion, and support proper movement patterns during joint motion and functional movements. Physical therapists with experience who treat individuals following MPFL injury will be aware of which manual techniques are safe, and which should be avoided, particularly after a surgical reconstruction.
Modalities. Your physical therapist may recommend therapeutic modalities, such as ice and heat, to aid in pain management.
Bracing. Compressive sleeves placed around the affected joint may help reduce pain and swelling. There are specific braces for individuals with too much kneecap motion that provide extra support through a buttress-like pad around the edge of the kneecap. In the event that surgery is required, braces may be used to control the amount of motion that is allowed as the postsurgical rehabilitation program progresses. For example, if an MPFL injury at the knee joint is treated surgically, a brace will keep the knee straight for the first several weeks after surgery.
Activity Guidance. Your physical therapist will help you return to activities in a safe and structured manner, using your symptoms as a guide to protect your knee joint as it heals. Your physical therapist will consider each stage of healing of the MPFL and recommend appropriate exercises to address your needs at each stage, and maximize the health of your knee joint.
If Surgery Is Required
When conservative management strategies are not successful in the treatment of MPFL injury, or in cases where there are other associated injuries, surgery may be considered. The goal of surgical intervention is to restore the integrity of the injured ligament, so that it can properly provide stability to the knee. There are many factors to consider when determining the appropriate surgical treatment, including the nature of your condition, your age, and your desired activity level. Your physical therapist will refer you to an orthopedic surgeon to discuss your surgical options.
If surgery is required to reconstruct your MPFL, you will spend several months in physical therapy after your surgery. Your physical therapist will help you progress through the stages of restoring normal range of motion, strength, and function. Rehabilitation following knee ligament surgeries is very important, as physical therapists are skilled at knowing when and how to progress patients safely after surgery. Your physical therapist will communicate closely with your surgeon to ensure that you are on track to a full recovery.
Can this Injury or Condition be Prevented?
Like many injuries and conditions, there are some factors that can be controlled and others that cannot when it comes to preventing MPFL injuries. In some cases, MPFL injuries are caused by a traumatic event, such as a sports injury. Occasionally, individuals with excessive joint or ligament looseness, or laxity, may suffer a nontraumatic MPFL injury; this may occur because the ligament has greater than normal flexibility and is not able to properly stabilize the knee joint during activities. Individuals who are involved in sports and other physical activities should make sure to properly strengthen their leg muscles to help support the structures around the knee joint. It is important to modify your activity and contact your physical therapist soon after you first feel pain.
Once you are involved in a rehabilitation program, your physical therapist will help you determine when you are ready to progress back to your previous activity level. Your physical therapist will make sure your body is ready to handle the demands of your activities, so that your injury does not return. That program will include guidance on which activities should be chosen and which should be avoided. You will also receive a program to perform at home that will help you maintain the improvements that you gained during rehabilitation.
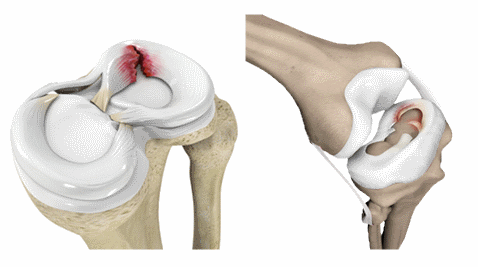
The meniscal tear is a common injury. It can affect athletes who play individuals and team sports. It's also common in people who have jobs that require lots of squatting, such as plumbers or coal miners. Your physical therapist can help you manage the injury and, if surgery is required, can help you prepare for the procedure and recover your strength and movement afterward.
A meniscal tear typically is caused by twisting or turning quickly on a bent knee, often with the foot planted on the ground. Although meniscal tears are common in those who play contact sports, anyone at any age can tear a meniscus. When people talk about having torn cartilage in their knee, they usually are talking about a meniscal tear.
Signs and Symptoms
When you tear a meniscus, you might:
- Feel a sharp, intense pain in the knee area
- Feel a "pop" or a tearing sensation
- Have difficulty walking because of pain or a "catching" sensation
- Have difficult straightening the knee
- Experience swelling within the first 24 hours of injury
How Is It Diagnosed?
Your physical therapist will:
- Conduct a thorough evaluation that includes a detailed review of your injury, your symptoms, and your health history
- Perform special tests to measure the range of motion (amount of movement) in your knee and determine which specific movements and positions increase your symptoms
- Use a series of tests that apply pressure to the meniscus to determine whether it appears to be damaged
The results of these tests may indicate the need for further diagnostic tests—such as ultrasound or magnetic resonance imaging—or a referral to an orthopedic surgeon for consultation.
How Can a Physical Therapist Help?
Your doctor may diagnose a torn meniscus, but meniscal injuries can often be managed without surgery. A short course of treatment provided by a physical therapist can help determine whether your knee will recover without surgery. The physical therapist plays an important role by controlling pain and swelling and by restoring full strength and mobility to your knee.
To control pain and swelling, your physical therapist may use ice and compression and will likely instruct you in the use of these treatments at home. Swelling is an important "guide" during your rehabilitation and can indicate when you are doing too much. Let your physical therapist know if you have an increase in swelling so that your program or activity level can be modified.
Your physical therapist may use a treatment called neuromuscular electrical stimulation (NMES) to help improve your strength. Your therapist also will design special exercises to maintain your strength during recovery and help restore full movement to the knee. You will be given a home program of exercises that are specific to your condition.
As you recover, your therapist will advise you on ways to maintain your fitness and activity level and will help you decide when you are ready to return to full activity.
If You Need Surgery
Patients with more serious meniscal tears, or those that don’t respond to a course of physical therapy, may need surgery. Surgically removing the torn cartilage (a procedure called a menisectomy) usually is a simple procedure that requires a brief course of physical therapy treatment. Most people are able to return to their previous level of activity, including sports, in fewer than 2 months.
Meniscus Removal
Following a simple menisectomy, your rehabilitation will likely be similar to that for nonsurgical injuries. Your physical therapist might use ice and compression to control pain and swelling and will show you how to use these treatments at home. Your therapist's focus will be on helping you get back your strength and movement through special exercises performed in the clinic and at home. Generally, you will need to use crutches or a cane, but only until you can walk without pain or a limp.
Meniscus Repair
Sometimes the surgeon will decide that the torn meniscus can be repaired, instead of removed. Research studies show that if a meniscal repair is possible, the long-term outcome is better than removal because the repair can reduce the risk of arthritis later in life.
Rehabilitation following a meniscal repair is slower and more extensive than with removal because the repaired tissue must be protected while it is healing. The type of surgical technique performed, the extent of your injury, and the preferences of the surgeon often determine how quickly you will be able to put weight on the leg, stop using crutches, and return to your previous activities.
After a meniscal repair, your physical therapist will help you control pain and swelling, help restore your strength, and help you regain full motion to the knee as soon as it is safe to do so. You'll have a program of exercises to do at home, and this program will be advanced as you improve. A brace may be used to help protect the repaired meniscus during the recovery phase. These braces usually allow you to fully straighten the knee but will limit your ability to bend it all the way, in order to prevent stress to the repair.
Returning to Activity
Whether your torn meniscus recovered on its own or required surgery, your physical therapist will play an important role in helping you return to your previous activities. Your therapist will help you learn to walk without a limp and go up and down stairs with ease.
If you have a physically demanding job or lifestyle, your therapist can help you return to these activities and improve how you do them.
If you are an athlete, you may need a more extensive course of rehabilitation. Your therapist will help you fully restore your strength, endurance, flexibility, and coordination to help maximize your return to sports and prevent reinjury. Return to sports varies greatly from one person to the next and depends upon the extent of the injury, the specific surgical procedure, the preference of the surgeon, and the type of sport. Your therapist will consider these factors when progressing your rehabilitation program and will work closely with your surgeon to help decide when it is safe for you to return to sports and other activities.
Can this Injury or Condition be Prevented?
There is little research at this time to support exercise or other interventions such as bracing for prevention of meniscal injuries. But we do know that you can make choices to help improve your overall fitness and help keep your knees as strong and as healthy as possible:
- Regular exercise helps strengthen the muscles that support your knees.
- Staying physically active helps prepare your body for the demands of a sport or strenuous activity.
- Although accidents are difficult to prevent, avoiding twisting or turning quickly while your foot is planted may help prevent meniscal tears.
If you already have knee problems, your physical therapist can help you develop a fitness program that takes your knees into account. Some exercises are better than others for those with a history of knee pain. Many exercises can be modified to fit your specific needs. For example, when performing exercises that include squatting, it’s important to make sure that your knee stays directly over your foot and doesn't twist or bend excessively.
Osteoarthritis of the knee (knee OA) is the inflammation and degeneration of the bones that form the knee joint (osteo=bone, arthro=joint, itis=inflammation). The diagnosis of knee OA is based on 2 primary findings: radiographic evidence of changes in bone health (through medical images such as x-ray and MRI) and an individual’s symptoms (how you feel). Approximately 14% of adults aged 25+ and 34% of adults aged 65+ are diagnosed with radiographic osteoarthritis. Specifically, about 16% of adults aged 45+ have knee OA.
What is Osteoarthritis of Knee?
Osteoarthritis of the knee (knee OA) is a progressive disease causing inflammation and degeneration of the knee joint that worsens over time. It affects the entire joint, including bone, cartilage, ligament, and muscle. Its progression is influenced by age, body mass index (BMI), bone structure, genetics, strength, and activity level. Knee OA also may develop as a secondary condition following a traumatic knee injury. Depending on the stage of the disease and whether there are associated injuries or conditions, knee OA can be managed with physical therapy. More severe or advanced cases may require surgery.
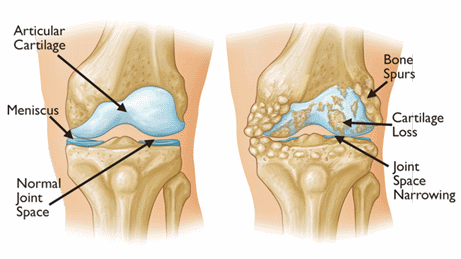
How Does it Feel?
Individuals who develop knee OA experience a wide range of symptoms based on the progression of the disease. Pain occurs when the cartilage covering the bones of the knee joint wears down. This narrows the space between the bones and causes friction. Because the knee is a weight-bearing joint, your activity level, and the type and duration of your activities usually have a direct impact on your symptoms.
Symptoms of knee OA may include:
- Worsening pain during or following activity, particularly with walking, climbing, or descending stairs, or moving from a sitting to standing position
- Pain or stiffness after sitting with the knee bent or straight for a prolonged period of time
- A feeling of popping, cracking, or grinding when moving the knee
- Swelling following activity
- Tenderness to touch along the knee joint
Typically these symptoms do not occur suddenly or all at once, but instead they develop gradually over time. Sometimes individuals do not recognize they have osteoarthritis because they cannot remember a specific time or injury that caused their symptoms. If you have had worsening knee pain for several months that is not responding to rest, it is best to seek the advice of a medical provider.
How Is It Diagnosed?
Knee OA is diagnosed by 2 primary methods. The first is based on your symptoms and a clinical examination. Your physical therapist will ask you questions about your medical history and activity routine. He or she will perform a physical exam to measure your knee's movement (range of motion), strength, mobility, and flexibility. You might also be asked to perform various movements to provoke the pain you are experiencing.
The second tool used to diagnose knee OA is diagnostic imaging. Your physical therapist may refer you to a physician, who will order x-rays of the knee in a variety of positions to assess the effect of weight-bearing (walking, standing, etc) on your knee joint. If more severe joint damage is suspected, an MRI may be ordered to look more closely at the overall status of the joint and surrounding tissues.
How Can a Physical Therapist Help?
Your physical therapist will design an individualized treatment program specific to the exact nature of your condition and your goals.
Range of Motion
Often, abnormal motion of the knee joint can lead to a progression of OA when there is more contact between, and wear on, the bones. Your therapist will assess your motion compared with expected normal motion and the motion of the knee on your uninvolved leg.
Muscle Strength
Strengthening the muscles around your knee will be an essential part of your rehabilitation program. Individuals with OA who adhere to strengthening programs have been shown to have less pain and an improved overall quality of life. There are several factors that influence the health of a joint: the quality of the cartilage that lines the bones, the tissue within and around the joints, and the associated muscles. Due to the wear and tear on cartilage associated with knee OA, maintaining strength in the muscles near the joint is crucial to preserve joint health. For example, as the muscles along the front and back of your thigh (quadriceps and hamstrings), cross the knee joint, they help control the motion and forces that are applied to the bones.
Strengthening the hip and core muscles also can help balance the amount of force on the knee joint, particularly during walking or running. The “core” refers to the muscles of the abdomen, low back, and pelvis. A strong core will increase stability through your body as you move your arms and legs. Your physical therapist will assess these different muscle groups, compare the strength in each limb, and prescribe specific exercises to target your areas of weakness.
Manual Therapy
Physical therapists are trained in manual (hands-on) therapy. Your physical therapist will gently move and mobilize your muscles and joints to improve their motion, flexibility, and strength. These techniques can target areas that are difficult to treat on your own. In patients with knee OA, the addition of manual therapy techniques to exercise has been shown to decrease pain and increase function.
Modalities
Your physical therapist may recommend therapeutic modalities, such as ice and heat, to aid in pain management.
Bracing
Compressive sleeves placed around the knee may help reduce pain and swelling. Devices such as realignment braces are used to modify the forces placed on the knee. These braces can help "unload" certain areas of your knee and move contact to less painful areas of the joint during weight-bearing activities.
Activity Recommendations
Physical therapists are trained to understand how to prescribe exercises to individuals with injuries or pain. Since OA is a progressive disease, it is important to develop a specific plan to perform enough activity to address the problem while avoiding increases in stress on the knee joint. Activity must be prescribed and monitored based on type, frequency, duration, and intensity, with adequate time allotted for rest and recovery. Your physical therapist will consider the stage and extent of your arthritis and prescribe an individualized exercise program to address your needs and maximize the function of your knee.
What if I Need Surgery?
In some cases of knee OA, the meniscus (shock absorber of the knee) may be involved. In the past, surgery to repair or remove parts or all of this cartilage was common. Current research, however, has shown in a group of patients who were deemed surgical candidates, 60-70% of those who participated in a physical therapy program, instead of surgery, did not go on to have surgery. Further, after 1 year those outcomes were unchanged. This study suggests that physical therapy may be an effective alternative for those patients who would like to avoid surgery.
Sometimes conservative management strategies are not successful. When these strategies fail surgical intervention such as arthroscopy or a total knee replacement, may be recommended. There are many factors to consider when determining the appropriate surgical treatment, including the nature of your condition, and your age, activity level, and overall health. Your physical therapist will refer you to an orthopedic surgeon to discuss your surgical options.
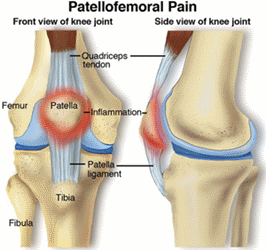
Patellofemoral pain syndrome (PFPS) is 1 of the most common types of knee pain, particularly among athletes, active teenagers, older adults, and people who do physical labor. Patellofemoral pain affects more women than men and accounts for 20%-25% of all reported knee pain.
What is Patellofemoral Pain?
Patellofemoral pain syndrome refers to pain at the front of the knee, in and around the kneecap. (The kneecap, or patella, is the triangle-shaped bone at the front of the knee joint. The pain usually is accompanied by tenderness along the edges of the patella.
Current research indicates that PFPS is an "overuse syndrome," which means that it may result from repetitive or excessive use of the knee. Other contributing causes may include:
- Weakness, tightness, or stiffness in the muscles around the knee
- An abnormality in the way the lower leg lines up with the hip, knee, and foot
These conditions can interfere with the ability of the patella to glide smoothly on the femur (the bone that connects the knee to the thigh) during movement. The friction between the under-surface of the patella and the femur causes the pain and irritation commonly seen in PFPS.
PFPS often occurs in people who are physically active or who have suddenly increased their level of activity, especially when that activity involves repeated knee motion, running, stair climbing, squatting, or repeated carrying of heavy loads. If you are older, you might have age-related changes that cause the cartilage on the under-surface of the patella to wear out. The result is pain and difficulty completing even the simplest daily tasks without pain.
Usually, patellofemoral pain is worse when you walk up or down hills or stairs and on uneven surfaces. This pain tends to increase with activity and improve with rest. You also may:
- Feel pain after sitting for long periods of time with the knee bent
- Occasionally hear or feel a "cracking" or "popping" when you bend or straighten your knee
How Is It Diagnosed?
Your physical therapist will review your health history, perform a thorough examination, and conduct a series of tests to evaluate the knee. Physical therapists use tests such as the patellar apprehension test, the Q-angle test, the patella alta test, and Clarke's sign (patellar grind test) to determine whether the patellofemoral joint is the source of pain.
In addition, your therapist may observe the alignment of your feet, analyze your walking and running patterns, and test the strength of your hip and thigh muscles to find out whether there is a weakness or imbalance that might be contributing to your pain. Finally, your therapist will check the flexibility of the muscles in your leg, paying close attention to those that attach at the knee.
Generally, x-rays are not needed to diagnose PFPS.
How Can a Physical Therapist Help?
After a comprehensive evaluation, your therapist will analyze the findings and prescribe an exercise and rehabilitation program just for you. Your program may include:
- Strengthening exercises targeted at the hip (specifically the abductor and rotator muscles of the buttock and thigh), the knee (specifically the quadriceps femoris muscle, which is located on the front of your thigh and straightens your knee), and the ankle
- Stretching exercises for the muscles of the hip, knee, and ankle
- Taping of the patella to reduce pain and retrain muscles to work efficiently
- Exercises for improving your performance of activities that have become difficult for you
If the alignment and position of your foot and arch appear to be contributing to your knee pain, your physical therapist may fit you with a special shoe insert called an orthosis. The orthosis can decrease the stress to your knee caused by excessive rotation or impact during walking and running.
If your pain is persistent, your physical therapist may:
- Have you try a lightweight brace
- Use pain-reducing treatments such as electrical stimulation
- Recommend that you apply ice or heat at home for relief
Your physical therapist will work with you to help you stay active and maintain your fitness level. You may need to modify your activity level or change your training activities until you recover; your therapist will show you how to do activities and exercises that will not increase your pain. Most important, your therapist can make recommendations to help prevent PFPS from returning.
Can this Injury or Condition be Prevented?
PFPS is much easier to treat if it is caught early. Report the first signs of knee pain to your physical therapist. Early treatment by a physical therapist may help stop the underlying problem before it gets worse. Your physical therapist also can help you adjust your daily activities and teach you exercises to do at home to strengthen your muscles and bones and help prevent PFPS from recurring.
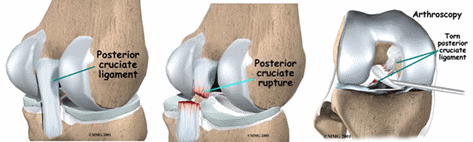
Posterior cruciate ligament (PCL) injury occurs when one of the ligaments on the inside of the knee is overstretched. Only 3% to 20% of knee ligament injuries are PCL injuries. Accidents, such as hitting the knee against the dashboard during a car collision, or falling onto a bent knee, are common causes of PCL injuries. Forceful straightening of the knee can also injure the PCL. Athletes who play sports, such as football and soccer, and skiers can experience PCL injuries. A newer source of PCL injury is the trend among dancers to land on the front of their shinbone from a high leap. Physical therapists treat PCL injuries to help reduce pain, swelling, stiffness, and any associated weakness in the knee or lower extremity.
Posterior Cruciate Ligament Injury
The posterior cruciate ligament (PCL) is a thick band of tissue deep inside the knee that connects the thighbone to the shinbone. The PCL prevents the shinbone from sliding too far backward under the thighbone. Any force that pushes the shinbone backward under the thighbone can cause a PCL injury. The PCL may be stretched, partially torn, or completely torn.
Knee injuries that tear the PCL often damage other ligaments or cartilage in the knee. A PCL injury can also break a piece of bone loose within the knee. PCL injuries can occur quickly—with a blunt force injury to the knee—or slowly, as the ligament is stressed over time.
How Does it Feel?
With an injured PCL, you may experience:
- Sharp or dull pain deep inside the knee joint or the back of the knee
- Pain in the knee when lifting a heavy load
- Pain when walking longer distances
- Swelling throughout the knee
- Stiffness in the knee
- A wobbly feeling in the knee
- Difficulty walking on the injured leg
- Difficulty going up or down stairs
- Difficulty when starting to run
PCL injuries sometimes do not cause a "popping" sound or sensation when they first occur, and for that reason, people may not be sure of the exact time of their injury.
How Is It Diagnosed?
If you see your physical therapist first, the therapist will conduct a thorough evaluation that includes taking your health history. Your physical therapist will also ask you detailed questions about your injury, such as:
- How and when did you notice the pain?
- Did you feel pain or hear a "pop" when you injured your knee?
- Did your knee straighten out very quickly, past its normal position?
- Did your knee get forcefully bent, past its normal position?
- Did you receive a direct hit to the leg while the knee was bent?
- Did you fall on a bent knee with the foot pointed downward?
- Did you see swelling around the knee in the first 2 to 3 hours following the injury?
- Does your knee feel like it is wobbling, locking, catching, buckling, or giving away when you try to use it?
Your physical therapist also will perform special tests to help determine the likelihood that you have a PCL injury. Your physical therapist will gently press on the front of your knee to determine if the ligament feels loose, and may perform additional tests to determine if other parts of your knee are injured. Your physical therapist will also observe how you are walking.
To provide a definitive diagnosis, your physical therapist may collaborate with an orthopedic physician or other health care provider, who may order further tests, such as an x-ray, to confirm the diagnosis and to rule out other damage to the knee, including fracture.
How Can a Physical Therapist Help?
Your physical therapist will work with you to design a specific treatment program that will speed your recovery, including exercises you can do at home. Physical therapy will help you return to your normal lifestyle and activities. The time it takes to heal the condition varies, but improvement is generally noted in 2 to 12 weeks.
During the first 24 to 48 hours following your injury, your physical therapist may advise you to:
- Rest your knee by using crutches or a brace, reducing the amount of weight you put on your injured leg, and avoiding any activity that causes pain.
- Apply ice packs to the area for 15– to 20 minutes every 2 hours.
- Consult with a physician for further services such as medication or diagnostic tests.
Your physical therapist will work with you over time to:
Reduce Pain and Swelling
Your physical therapist may use a variety of treatments and technologies to control and reduce your pain and swelling, which may include ice, heat, ultrasound, electrical stimulation, taping, exercises, and hands-on therapy, such as massage.
Improve Motion
Your physical therapist will choose specific activities and treatments to help restore normal movement in the knee and leg. These might begin with passive motions that your physical therapist performs for you to gently move your leg and knee joint, and progress to active exercises and stretches that you do yourself.
Improve Flexibility
Your physical therapist will determine if any of your leg muscles are tight, and teach you how to stretch them with gentle exercise.
Improve Strength
Certain exercises will aid healing at each stage of recovery; your physical therapist will choose and teach you the correct exercises and equipment to steadily restore your strength and agility. These may include the use of cuff weights, stretch bands, weight-lifting equipment, and cardio-exercise equipment, such as treadmills or stationary bicycles.
Improve Balance
Regaining your sense of balance is important after an injury. Your physical therapist will teach you exercises to improve your balance skills.
Restore Agility
Speed and accuracy of leg movement is important in athletic activities. Your physical therapist will help you regain these skills in preparation for a return to sports activities.
Speed Recovery Time
Your physical therapist is trained and experienced in choosing the best treatments and exercises to help you heal, return to your normal lifestyle, and reach your goals faster than you are likely to do on your own.
Your physical therapist will work with you to set your work, sport, and home-life recovery goals. Your treatment program will help you reach those goals in the safest, fastest, and most effective way possible. Your physical therapist will teach you exercises, work retraining activities, and sport-specific techniques and drills to help you return to your regular activities.
If Surgery Is Necessary
Surgery is not usually required to treat a mild PCL injury. However, it may be needed if:
- The PCL is completely torn
- A piece of bone has broken loose
- There are other ligament injuries
- You constantly feel like your knee is going to buckle beneath you
Athletes may elect to undergo surgical replacement of the PCL to improve the stability of the knee during sports activities. If other parts of the knee are injured at the same time as the PCL, you may need different treatment for those injuries, including surgery. If surgery is needed, you will follow a recovery program over several weeks guided by your physical therapist. Your physical therapist will help you minimize pain, regain motion and strength, and return to normal activities in the speediest manner possible.
Can this Injury or Condition be Prevented?
Your physical therapist can recommend a home-exercise program to strengthen and stretch the muscles around your knee, upper leg, and abdomen to help prevent future injury. These may include strength and flexibility exercises for the leg, knee, and core muscles.
To help prevent a recurrence of the injury, your physical therapist may advise you to:
- Always use a seat belt to help prevent injury during a car accident.
- Position your car seat so it is not too close to the dashboard.
- Avoid intentionally landing on the front of your shinbone or on your knees.
- Always warm up before starting a sport or heavy physical activity.
- Maintain or improve sport-specific conditioning and techniques that are right for your level of sport activity.
- Wear shoes that are in good condition and fit well.
- Maintain a healthy weight.
