-
 Injury keeping you out of the game?Our experts will get to the core of your fitness needs.OUR SERVICES
Injury keeping you out of the game?Our experts will get to the core of your fitness needs.OUR SERVICES -
 GET BACK TO THE ACTIVITIES YOU LOVEOUR SERVICES
GET BACK TO THE ACTIVITIES YOU LOVEOUR SERVICES -
 RESTORING YOUR PHYSICAL ABILITYOUR SERVICES
RESTORING YOUR PHYSICAL ABILITYOUR SERVICES -
 RESTORING YOUR QUALITY OF LIFEOUR SERVICES
RESTORING YOUR QUALITY OF LIFEOUR SERVICES -
 EVIDENCE BASED PRACTICEOUR SERVICES
EVIDENCE BASED PRACTICEOUR SERVICES -
 APPROPRIATE PROGRAM FOR A SUCCESSFUL RECOVERYOUR SERVICES
APPROPRIATE PROGRAM FOR A SUCCESSFUL RECOVERYOUR SERVICES -
 HELPING YOU ACHIEVE YOUR GOALSOUR SERVICES
HELPING YOU ACHIEVE YOUR GOALSOUR SERVICES
Wrist and Hand
A wrist fracture is a break in one of the bones near the wrist. In the United States, 1 out of every 10 broken bones diagnosed is a wrist fracture. Injury can occur as a result of a trauma, such as falling while playing sports or simply tripping when walking down a sidewalk. Children are susceptible to wrist fractures because of the high-risk sports they commonly play. A child may sustain a wrist fracture falling off a bike, playing football or soccer, or falling off playground equipment. Wrist fractures are also common in women after menopause, and frequently occur in the elderly population due to falls. A physical therapist can help individuals who have sustained a wrist fracture regain normal wrist motion, strength, and function, and learn how to prevent future fractures.
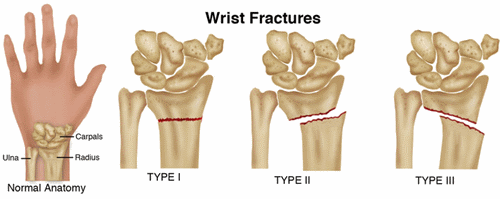
A fracture is a crack or a break in a bone. Wrist fractures due to falls happen most often when people stretch the arm straight out to catch themselves as they fall. The wrist is made up of 8 small bones called carpal bones, and 2 bones in the forearm called the radius and the ulna. A wrist fracture is diagnosed when any of those bones breaks or cracks. The most frequently fractured bone is the radius, the bone in the forearm that is closest to the thumb.
There are 3 types of bone fractures:
- Type 1 – a "nondisplaced" fracture, where the bone is broken but is still in a normal position.
- Type 2 – a fracture where a fragment of bone is shifted from its normal position.
- Type 3 – the most serious type of fracture, with multiple breaks of the bone or bones.
Type 1 and 2 fractures usually are treated without surgery. Type 3 fractures, however, usually require surgery.
How Does it Feel?
A fractured wrist is usually painful and movement is affected. If you have sustained a wrist fracture, you may experience:
- Pain in the area of the fracture, which could be anywhere in the wrist, depending on which bone was affected. The pain can radiate from the wrist into the fingers, and even into the forearm.
- Swelling in the wrist and possibly in the hand, usually on the top surface of the wrist and hand.
- Tenderness to touch in the wrist.
- Difficulty and pain when moving the wrist or fingers
How Is It Diagnosed?
An x-ray is the best way to diagnose a wrist fracture. If you have sustained a fall and are experiencing any of the symptoms mentioned above, you need to visit an emergency room, an urgent-care center, or your physician to get a complete diagnostic x-ray.
If a physical therapist suspects that you have a wrist fracture, the therapist may arrange for an x-ray and refer you to an appropriate physician. Your physical therapist can check for damage to other joints and muscles, and make sure that the nerves and blood vessels in your wrist, forearm, and hand have not been affected by the broken bone. In most cases, people with fractures visit a physician with a specialty in managing bones and joints (an orthopedist). Depending on the type of fracture, the physician might prescribe a cast or a sling to immobilize the area for a period of time until the fracture is healed. The amount of healing time varies, depending on the individual and the type of fracture, and can be anywhere from 4 to 10 weeks. If the fracture is severe, surgery will be required. The recovery time may be longer following surgery, depending on the severity of the injury.
How Can a Physical Therapist Help?
Your physical therapist will work with you following a wrist fracture to help you regain normal wrist motion, strength, and function, and will provide education and training to help you prevent future fractures.
While Your Wrist Is In a Cast or a Sling
While your bone heals, your arm will be in a cast or a sling to keep it still and promote healing. During that time, it is important to ensure that the arm does not get too stiff, weak, or swollen. Depending on the amount of activity that is allowed for your type of fracture, your physical therapist will prescribe gentle exercises to keep your shoulder, elbow, and fingers moving while you are in the cast or sling.
Most people with wrist fractures will slowly return to exercising the other arm and the legs, so that the rest of the body doesn't get out of shape while the fracture is healing. Your physical therapist can help you adapt your exercise program, so that you can maintain your overall strength and fitness without interfering with the healing of your wrist.
When the Cast or Sling Is Removed
After your cast or sling is removed, your wrist will most likely be stiff, and your arm will feel weak. Your physical therapist will examine your wrist, and select treatments to improve its function and restore strength to your arm.
Your rehabilitation will include treatments to:
Reduce Pain. Your physical therapist might use either warm or cold therapeutic treatments, or electrical stimulation, to help control pain or swelling in your wrist, hand, or arm.
Relieve Stiffness. Your physical therapist may use skilled hands-on techniques (manual therapy) to enable your joints and muscles to move more freely with less pain.
Increase Your Strength and Ability to Move. Physical therapists prescribe several types of exercises during recovery from a wrist fracture. Early on, your physical therapist can help you begin to gently move your elbow, using "passive range-of-motion" exercises. As your arm gets stronger, you can exercise it yourself without weights ("active range-of-motion" exercises). Once the bone is well-healed, you can begin to perform resistance exercises, using weights or elastic bands. In addition to prescribing range-of-motion and strengthening exercises, your physical therapist can help you retrain your muscles to react quickly when you need to protect yourself from a fall.
Get Back to Your Daily Activities. Your physical therapist will help you remain independent by teaching you how to perform your daily activities (eg, dressing, working on a computer, and cooking), even while wearing a cast or a sling. Once you can move your arm freely without pain, your physical therapist may begin adding activities that you were doing before your injury, such as using your arm for dressing, grooming, and housekeeping. Your physical therapist will design your individualized program based on an examination of your wrist, goals, level of physical activity, and general health.
Prepare for More Demanding Activities. Depending on the requirements of your job or the type of sports you play, you might need additional physical therapy tailored to meet specific demands. Your physical therapist will develop a specialized program to address your unique needs and goals.
Prevent Long-Term Disability. Everything your physical therapist prescribes for you will help prevent long-term disability by:
- Returning the arm to a strong level of fitness.
- Restoring full movement and strength in a safe manner, while healing occurs.
- Assessing the fracture to make sure that you can return safely to previous home and work activities.
- Guiding you to a safe return to sports and other physical activities. A return too early after a fracture may increase the risk of another fracture.
- Recommending protective equipment, such as wrist guards, for use during sports.
Can this Injury or Condition be Prevented?
In addition to helping individuals prevent long-term disability following a wrist fracture, physical therapists can help different at-risk populations prevent fractures.
- For the aging population, avoiding falls and other trauma is the best way to prevent fractures. Physical therapists are experts at determining your risk of falling, and can teach you how to perform balance exercises and take precautions to avoid falls. They also can perform work and home safety evaluations to make sure that your daily environment is safe.
- For postmenopausal women with osteoporosis leading to a higher risk of wrist fracture, a physical therapist can teach weight-bearing exercises to help build stronger bones. Your physical therapist also may refer you to a nutritionist for vitamin D supplements or other dietary changes to help make your bones stronger. Education in proper posture and body mechanics and joint protection techniques can be helpful in preventing strain on the wrist and arms.
- For children, wearing proper protective gear, such as wrist guards, can reduce the risk of a wrist fracture when playing certain sports. Making sure that playground equipment your child uses is safe and built on a soft surface can also reduce the risk of wrist fractures due to falls.
Wrist tendinitis is a condition where 1 or more tendons in the wrist become inflamed and irritated. There are several tendons in the wrist that connect the muscles of the forearm and hand to the bones of the wrist and hand. These tendons are the small rope-like structures that you can see connecting to the fingers on the back of your hand. There are a number of conditions that can affect the tendons in this area.
- Wrist tendinitis applies to the early stages of tendon inflammation and irritation.
- Tendinopathy is the name given to the condition when it persists over time, is not treated, and becomes chronic.
- Tenosynovitis is the term given to an irritation that develops when the synovial sheath (through which some of these tendons glide) thickens and restricts the tendon.
- De Quervain's Tendinitis applies to tendinitis that develops on the thumb side of the wrist.
Wrist tendinitis is a condition that most commonly occurs in individuals who perform repetitive activities using the hand and arm. These include computer users, factory workers, and athletes who throw and catch balls and play racquet sports. In the United States, the incidence of tendinitis as an occupational injury in people who work full time is 1.1 per 100,000. Overuse tendinitis is responsible for 25% to 50% of all sports injuries in the United States. Older individuals are often more at risk for wrist tendinitis due to a loss of elasticity in the wrist tendons. Physical therapists help people with wrist tendinitis reduce their pain, increase their wrist flexibility and strength, and return to their previous functional activities and sports.
How Does it Feel?
Several tendons in the wrist can become irritated with wrist tendinitis. Pain symptoms associated with the condition include:
- Pain where the arm meets the hand, which can radiate up into the elbow.
- Pain on the thumb side of the wrist (radial) or the little-finger side of the wrist (ulnar).
- Pain that only occurs when the wrist is under strain, which can become constant pain when left untreated.
- Pain when putting pressure on the hand, such as using the arms to push yourself up out of a chair to stand.
Besides pain, other symptoms include:
- Stiffness of the wrist, and a decreased ability to bend and extend the wrist.
- Inflammation or swelling in the wrist area.
- Tenderness to touch in the wrist and/or forearm muscles.
How Is It Diagnosed?
Your physical therapist will conduct a thorough evaluation of your entire arm to include the shoulder, elbow, wrist, and hand. The therapist will ask you to describe the types of activities you normally perform using your arm at home, at work, and for recreation, and which of these activities causes pain or stiffness in the area. You will be asked how long the pain has been occurring and how it is affecting your regular activities of daily living. Your physical therapist will check your range of motion and strength in your entire upper arm. Your therapist will gently touch specific areas of your wrist and forearm to determine which wrist tendons are involved, and check for any swelling in the area.
How Can a Physical Therapist Help?
Physical therapy is a highly effective treatment for wrist tendinitis. You will work with your physical therapist to devise a treatment plan that is specific to your condition and goals. Your individual treatment program may include:
Pain Management. Your physical therapist will help you identify and avoid painful movements, and show you how to correct abnormal postures to reduce stress on the wrist. Your therapist may recommend resting the wrist short-term, and applying ice to the area to help alleviate pain. Your physical therapist also may apply a wrist brace to restrict wrist movement, allowing the tendons to heal.
Manual Therapy. Your physical therapist may use manual techniques, such as gentle joint movements, soft-tissue massage, and wrist stretches to get your wrist moving properly.
Range-of-Motion Exercises. You will learn exercises and stretches to reduce stiffness and help your wrist, hand, and forearm begin to move properly.
Strengthening Exercises. Your physical therapist will determine which strengthening exercises are right for you, depending on your specific areas of weakness. The entire arm, including the shoulder, elbow, and wrist, can potentially be weakened and contribute to the movement dysfunction that causes tendinitis. Your physical therapist will design an individualized home-exercise program to meet your specific needs and goals, which you can continue long after you have completed your formal physical therapy.
Patient Education. Depending on the specific activities you plan on resuming, your physical therapist will teach you ways to perform actions, while protecting your wrist and hand. For example, keeping the wrist in a neutral position to reduce excessive force while performing repetitive tasks, and taking frequent breaks are ways to decrease your chances of reinjury.
Functional Training. As your symptoms improve, your physical therapist will teach you how to correctly perform functional movement patterns using proper wrist mechanics, such as typing on a computer or swinging a racquet. This training will help you return to pain-free function on the job, at home, and when playing sports.
Can this Injury or Condition be Prevented?
To prevent wrist tendinitis, physical therapists recommend that you:
- Avoid repetitive wrist and hand movements.
- Warm up the muscles around the wrist and hand before starting an activity.
- Perform regular stretches to maintain flexibility in the wrist and forearm before and after exercise or activity.
- Perform regular upper-body strengthening exercises to enable the wrist and hand to tolerate sports and other activities of daily living, with less stress to the joint.
- Follow joint protection techniques when using the wrist, such as balancing rest with work, and using the larger muscles of the arm for heavier tasks.
- Do not continue an activity that is painful or uncomfortable to the wrist and hand.
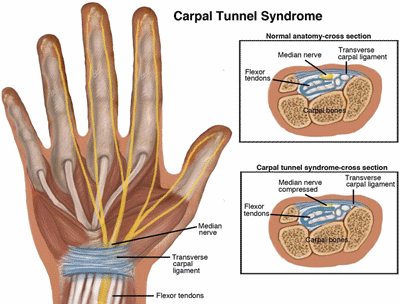
Carpal tunnel syndrome (CTS) is a common condition of the wrist and hand that can affect the use of the whole arm. It is caused by pressure on the nerve at the base of the palm (median nerve). Because of the demands that people place on their hands and wrists, CTS is a common condition affecting 1 out of 20 Americans. Surgery for this condition is commonly performed on the wrist and hand. Fortunately for most people who develop CTS, physical therapy treatment can often relieve pain and numbness and restore.
What is Carpal Tunnel Syndrome?
About the width of your thumb, the carpal tunnel is a narrow channel on the palm side of your wrist. The tunnel protects the median nerve and the tendons that bend your fingers. Pressure on the nerve can cause pain and weakness in your wrist and hand and numbness or tingling in some of your fingers. This pressure is caused by crowding or irritation of the median nerve in the carpal tunnel and can lead to CTS.
normal use of the hand, wrist, and arm without the need for surgery.
Extreme wrist positions, as well as a lot of finger use, especially with a lot of force or vibration (such as holding the steering wheel when driving heavy machinery), can all contribute to CTS.
CTS is common in professions such as assembly-line work, particularly meat packing; and jobs requiring the use of hand tools, especially tools that vibrate. Although excessive keyboard and computer use is often associated with CTS, those performing assembly line work are 3 times more likely to develop CTS than those who perform data entry work. Some leisure activities can also create CTS, such as sewing, sports such as racquetball and handball, and playing string instruments such as the violin.
The following health conditions can also lead to CTS in some individuals:
- Inflammation and swelling of the tendons of the wrist
- Injuries to the wrist (strain, sprain, dislocation, fracture)
- Hormone or metabolic changes (pregnancy, menopause, thyroid imbalance)
- Fluid retention (eg, during pregnancy)
- Diabetes
- Certain medicine use (eg, steroids)
- Degenerative and rheumatoid arthritis
Signs and Symptoms
CTS usually starts gradually, with symptoms such as burning, tingling, "pins and needles," or numbness in the palm of the hand and fingers. Often the symptoms are more noticeable during the night, and individuals often report being wakened with symptoms. Many people feel the need to "shake out" their hands to try to relieve the symptoms.
As the condition progresses, the symptoms are noticed during the daytime and are often worse when holding items such as a heavy book or a hairbrush. Weakness of the hand and more constant numbness may occur if the pressure on the nerve continues. You may find that you drop objects unexpectedly or have a weakness in your grip.
How Is It Diagnosed?
Physical therapists work closely with other health care professionals to accurately diagnose and treat CTS. Symptoms of CTS are typical, and it is often possible to diagnose it without extensive testing. Physical therapists are experts in the movement and function of the body and will conduct an evaluation to determine all of the factors that may be contributing to your condition.
These are several tests that may be used to help diagnose CTS:
- Examination of your neck and entire upper extremity to rule out other conditions. Many patients have been told they have CTS, only to find out that the pain is coming from another body area.
- Grip strength of fingers and thumb
- Sensory tests
- Wrist and hand range-of-motion
- Wrist flexion (Phalen) test: Your physical therapist will have you push the backs of your hands together for 1 minute. Tingling or numbness in your fingers that occurs within 60 seconds may be an indication of CTS.
- Tinel's Sign: Your physical therapist will use a reflex hammer or finger to tap over the median nerve at your wrist. Tingling in the thumb and index and middle fingers may indicate CTS.
- Electrical studies (electromyogram/EMG) and nerve conduction velocity (NCV): These tests determine the transmission of the nerve and the severity of the CTS.
- X-rays: When trauma has occurred or if there is reason to suspect anatomical abnormality, x-rays may be ordered.
In some cases, your physical therapist may refer you to a physician or other health care professional for additional testing or treatment.
How Can a Physical Therapist Help?
After the evaluation, your physical therapist will prescribe your treatment plan based on your specific case.
Conservative Care
If your evaluation confirms early-stage CTS, conservative care will be recommended as a first step. Physical therapy treatment can be effective in reducing your symptoms and getting you back to performing normal activities. During your first visit with the physical therapist, be prepared to describe your symptoms in as much detail as possible, and say what makes your symptoms worse.
Depending upon the causes of your CTS, your therapy program may include:
- Education regarding:
- changing wrist positions (ie, avoiding prolonged bent wrist positions)
- proper neck and upper back posture (ie, avoiding forward head or slouching)
- safe use of sharp utensils, tools, or other implements, if sensory changes are identified
- "stretch breaks" during your work or daily routine
- Exercises to increase the strength of the muscles in your hand, fingers, and forearm—and in some cases, the trunk and postural back muscles
- Stretching exercises to improve the flexibility of the wrist, hand, and fingers
- Use of heat/cold treatments to relieve pain
- Use of a night splint to reduce discomfort
- A worksite visit to assess your work area. For example, if you sit at a desk and work on a computer, it's important for the keyboard to be in proper alignment to help avoid working in a bent wrist position.
- Increasing the size of tool and utensil handles by adding extra material for a more comfortable grip
- Anti-vibration gloves or anti-vibration wraps around tool handles, if vibration is a factor at your workplace
Your physical therapist will also consider your home and leisure activities, with recommendations such as wearing gloves to keep the wrist/hands warm and limiting sports that aggravate the condition, such as racquet sports, until symptoms resolve.
The goals of physical therapy are to reduce your symptoms without the need for surgery, to enable you to be as active and functional as possible, and to help you resume your normal work, home, and leisure activities.
Physical Therapy Following Surgery
If the evaluation reveals that your CTS is more severe, or if your symptoms persist, your physical therapist may refer you to a physician for a surgical consultation. If necessary, surgery will be performed to release the band of tissue that is causing pressure on the median nerve. Physical therapy treatment is important after surgery to help restore strength to the wrist and to learn to modify habits that may have led to symptoms in the first place. Your physical therapy treatment may include:
- Exercises to improve the strength of the wrist/hand muscles and improve function
- Stretching to improve mobility of the wrist/fingers and improve function
- Scar management to keep the skin supple and flexible
- Education regarding appropriate posture and wrist position to avoid carpal tunnel compression in home/leisure activities
- A worksite visit or simulation to optimize postures and positions
Can this Injury or Condition be Prevented?
There are no proven strategies for preventing CTS, but there are ways to minimize stress to your hands and wrists. Since there are contributing factors to developing CTS, one single solution may not be effective.
The following strategies are effective ways to minimize stress to your hands and wrists:
- Reduce force. Most people use more force than needed when performing work with their hands. Relax your grip to avoid muscle fatigue and strain. For prolonged handwriting, use a larger-handle pen or soft gel grip.
- Take frequent breaks. When doing repeated activities, give your hands a break by performing stretching exercises once in a while. If possible, alternate your hands when completing some tasks.
- Neutral wrist position. Avoid bending your wrists by keeping them in a straight or “neutral” position. This means your wrist should not be bent up (extended) or down (flexed).
- Work area adjustment. Have a physical therapist examine your work area to make sure it fits your height, posture, and the tasks required. Simple adjustments can help avoid unnecessary strain.
- Improve your posture. Make sure your posture is appropriate to the task you are performing. Believe it or not, proper alignment of your trunk, neck, and shoulders can prevent excessive strain and improper positioning of the wrists and hands.
- Keep your hands warm. You are more likely to develop hand pain and stiffness if you work in a cold environment. If you can't control the temperature, be sure to wear gloves to keep your hands and wrists warm.
- Maintain good health. Paying attention to your general health is an important step in preventing CTS. Staying physically fit and maintaining a healthy weight may help control diseases and conditions that may contribute to the onset of CTS.
De Quervain's (dih-kwer-VAINS) tendinitis is a condition that causes pain and tenderness at the thumb side of the wrist, at the base of the thumb and forearm. Pain is worsened with grasping or extending the thumb (pulling it back like "thumbing a ride"). People of all ages can develop this condition, which usually happens when the tendons are strained by prolonged or repetitive use of the hand, rapid or forceful hand use, or use of the hand or arm in an awkward position. Tendons at the wrist become irritated and thickened, resulting in pain when moving the thumb and grasping objects. Common forms of treatment for De Quervain’s include splinting and range-of-motion exercises. Injection for cortisone by a doctor is common treatment. Persistent cases may require surgery.
De Quervain's tendinitis is a common condition involving tendons of the wrist. Tendons are tough cords or bands of connective tissue that attach muscles to a bone. The thumb and wrist extensor tendons (Abductor Pollicus Longus and Extensor Pollicus Brevis) are encased in a "sheath" or a tunnel at the wrist, which keeps the tendons in place.
De Quervain's tendinitis can occur gradually or suddenly, when the tendons become inflamed or thickened from overload or repetitive use, and have difficulty sliding through the extensor tunnel.
Risk factors for developing De Quervain's tendinitis include:
- Chronic overuse of the hand.
- Excessive use of the thumb from texting and gaming.
- Being female (women are 8 to 10 times more likely to develop this condition than men).
- Pregnancy.
- Using the hand or arm in a position that feels awkward.
- Participation in sports that stress the hand and wrist, such as golf and tennis.
- Age greater than 40 years.
- Race; members of the black community may be more likely to experience this problem.
How Does it Feel?
A person who has De Quervain's tendinitis may:
- Feel localized tenderness, pain, and, swelling at the wrist near where the thumb is attached to the forearm.
- Have difficulty pinching or grasping with the thumb or hand.
- Feel pain when moving the wrist from side to side or twisting it.
- Experience limited motion and feeling of weakness in the thumb.
- Have difficulty flexing the thumb.
- Notice a "catching" or "snapping" sensation with movement of the thumb (a less common symptom).
Active use of the hand with activities, such as writing, opening jars, lifting a child, hammering, sports, and any workplace or home activity that involves pinching or grasping with the thumb, can provoke the symptoms of pain, stiffness, and weakness.
Note: Other conditions of the wrist and hand can cause symptoms similar to those stated here. Your physical therapist will help to identify any underlying problems of your joints, tissues, or nerves that may be causing similar symptoms.
How Is It Diagnosed?
Your physical therapist will ask you how and when you first experienced symptoms, and what it feels like at the present time. Your therapist will perform a physical exam that will include feeling for tender spots, measuring the flexibility and range of motion of the thumb and wrist, and testing the strength of the thumb muscles and grip. Your physical therapist will also perform a Finkelstein test, which gently stretches the tendons on the thumb side of the wrist through the extensor tunnel. Pain during this test is common with De Quervain’s tendinitis.
Your physical therapist will also perform other tests to rule out any underlying conditions that may mimic De Quervain's symptoms.
How Can a Physical Therapist Help?
If your physical therapist confirms De Quervain’s Tendinitis from an evaluation, they will work with you to develop an individualized plan with you for this condition.
Your physical therapist will review and evaluate how you use your hand and wrist for functional activity. The review will include your daily activities, work, and sports activities. The physical therapist will try to help you identify what activities or positions that you use that may contribute to the problem. They will instruct you how to make changes in your function to help healing and reduce risk of the problem in the future.
Specific instructions may include avoiding repetitive thumb and/or wrist movements, avoid flexing the thumb, and avoid moving the hand toward the pinkie finger as much as possible. You should also avoid forceful hand movements, and any movements or activities that increase pain.
The therapist may provide a wrist splint to position your wrist and thumb for rest, and to provide compression to help pain and swelling.
Your therapist may also work with you to reduce pain and inflammation.
Ultrasound therapy may be applied to improve pain. This treatment uses ultrasonic sound waves applied over the involved area to improve circulation, reduce swelling, and aide healing of the tissues and tendons.
Iontophoresis is another option to reduce swelling and pain. Iontophoresis is a type of electrical stimulation that is used to administer medication to the problem area through your skin.
Ice or heat may be recommended for short term pain relief. Your therapist will advise you for what is best for your condition.
Exercise is prescribed to improve range of motion and prevent stiffness. Early on, exercise is restricted to avoid aggravating the condition. As the condition improves, exercises will be progressed to improve strength for functional activity, as well as improve active range of motion of the thumb and wrist.
If your symptoms do not respond to conservative care, your physical therapist will refer you to a physician who will determine if you need medication, injection, or surgical care for further recovery.
How Can a Physical Therapist Help Before & After Surgery?
If your De Quervain's problem does require surgery, your physical therapist may fit a splint to your hand and wrist after the procedure. Your physical therapist will help you to control any swelling, maintain and improve your hand and wrist flexibility, build your strength, and improve your range of motion, allowing you to safely return to your preinjury activity levels.
Can this Injury or Condition be Prevented?
It may be possible to prevent De Quervain's tendinitis. Some risk factors cannot be controlled, such as gender, race, or age; however, physical therapists recommend that you:
- Avoid chronic overuse of the hand.
- Avoid or restrict overly forceful use of the wrist.
- Avoid excessive use of the thumbs for texting and gaming.
- Avoid putting the wrist and hand in awkward positions while using the hand or arm.
- Train and condition in sports, such as golf and tennis to minimize wrist and thumb strain.
Your physical therapist can teach you correct and safe hand and wrist positions to maintain during your daily home, work, and sport activities.
ho2 Goes Here
hc2 Goes Here
hs2 Goes Here
ht2 Goes Here
ho2 Goes Here
hc2 Goes Here
hs2 Goes Here
ht2 Goes Here
ho2 Goes Here
hc2 Goes Here
hs2 Goes Here
ht2 Goes Here
ho2 Goes Here
hc2 Goes Here
hs2 Goes Here
ht2 Goes Here
ho2 Goes Here
hc2 Goes Here
hs2 Goes Here
ht2 Goes Here
ho2 Goes Here
hc2 Goes Here
hs2 Goes Here
ht2 Goes Here
